Ethide, Ethionamide
- Introduction to Ethide (Ethionamide)
- Composition and Active Ingredients
- How Ethide (Ethionamide) Works
- Approved Uses of Ethide (Ethionamide)
- Off-Label Uses of Ethide (Ethionamide)
- Dosage and Administration Guidelines
- Common Side Effects of Ethide (Ethionamide)
- Serious Side Effects and Adverse Reactions
- Drug Interactions with Ethide (Ethionamide)
- Contraindications and When Not to Use Ethide (Ethionamide)
- Important Precautions Before Taking Ethide (Ethionamide)
- Special Considerations for Specific Populations
- Administration to Pregnant Women and Nursing Mothers
- Administration to Children and Adolescents
- Handling Precautions and Safe Storage
- Overdosage and Toxicity Management
- Conclusion and Final Recommendations
Introduction to Ethide (Ethionamide)
Overview of Ethide and Its Classification as a Second-Line Anti-Tuberculosis Drug
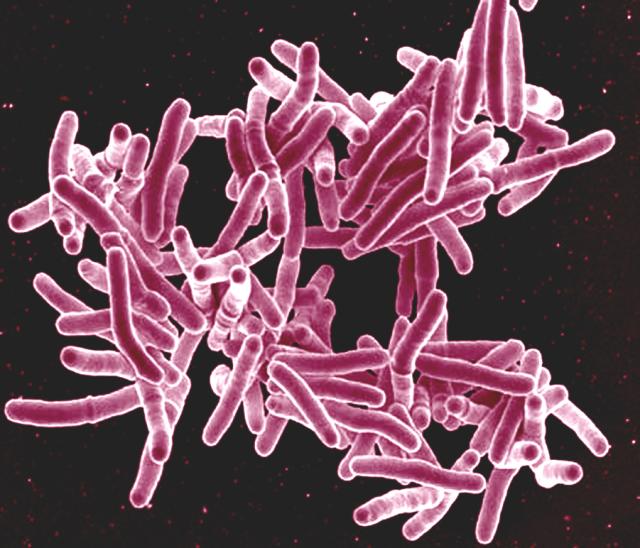
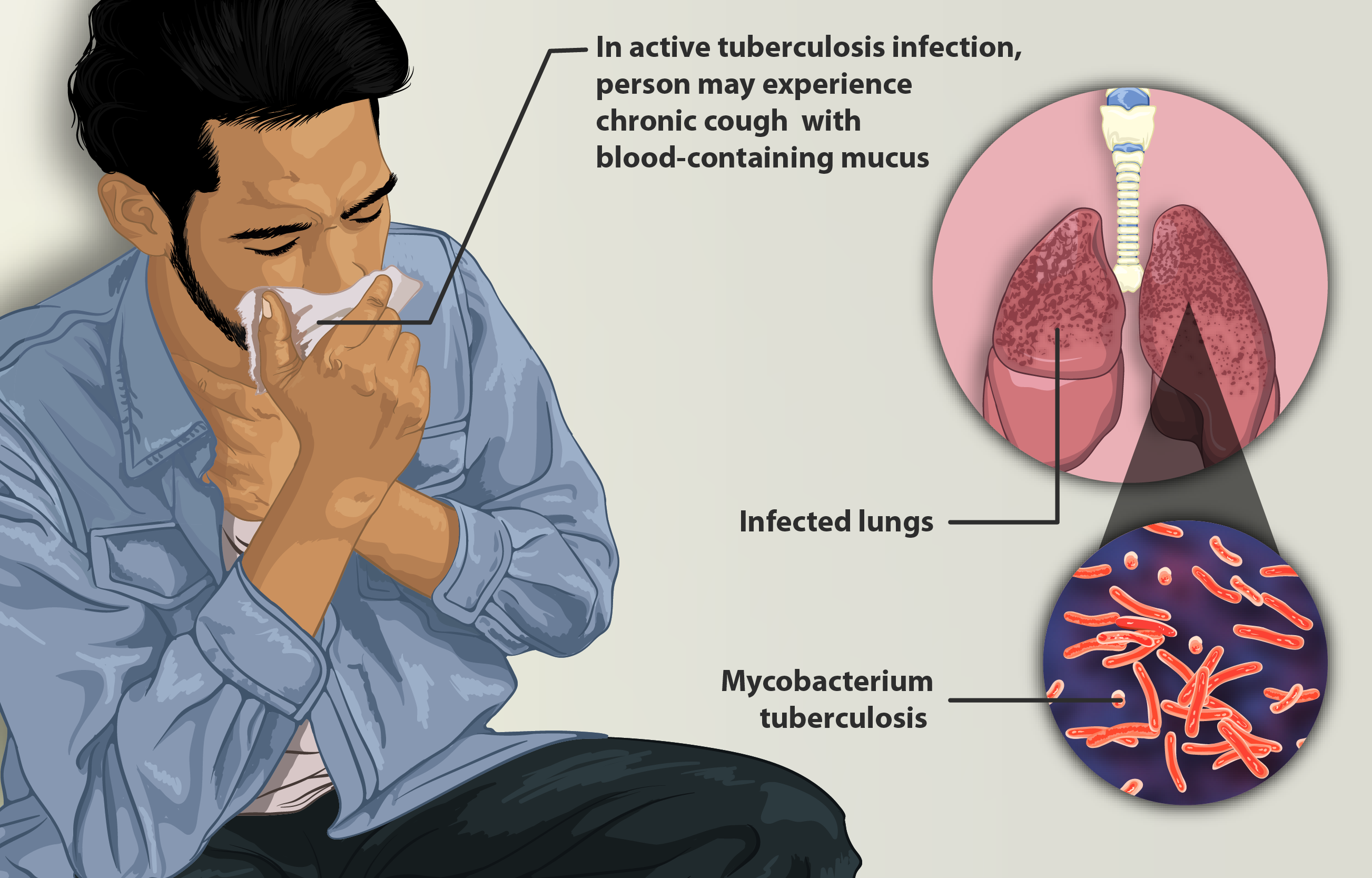
Ethide or Ethionamide is a medication used to treat tuberculosis when initial treatments are ineffective or when resistance, to common TB drugs develops. It is similar in structure to isoniazid. Ethionamide works by interfering with biochemical processes, in Mycobacterium tuberculosis to inhibit its growth.
Historical Development and FDA Approval Status
Ethionamide was first developed in the middle of the century as a medication, for treating tuberculosis when resistance to treatments was on the rise. In the 1960s the U.S. Food and Drug Administration (FDA) approved it for use in treating multidrug tuberculosis (MDR-TB) securing its position, in the realm of TB treatment. Despite its effectiveness it is used cautiously because of its side effects.
Mechanism of Action
Ethionamide acts as a prodrug that needs activation inside the cell. After being metabolized it hinders the synthesis of acid, an important element in the mycobacterial cell wall. This interference results, in heightened cell permeability and the breakdown of integrity leading to bacterial demise.
Role in Multidrug-Resistant Tuberculosis (MDR-TB) Treatment
Multidrug-resistant tuberculosis poses a health issue worldwide. The use of Ethide plays a part, in addressing MDR-TB cases where resistance, to rifampicin and isoniazid, has been identified. Doctors include Ethionamide in treatment plans to enhance the killing of bacteria and reduce the likelihood of additional resistance emerging.
Composition and Active Ingredients
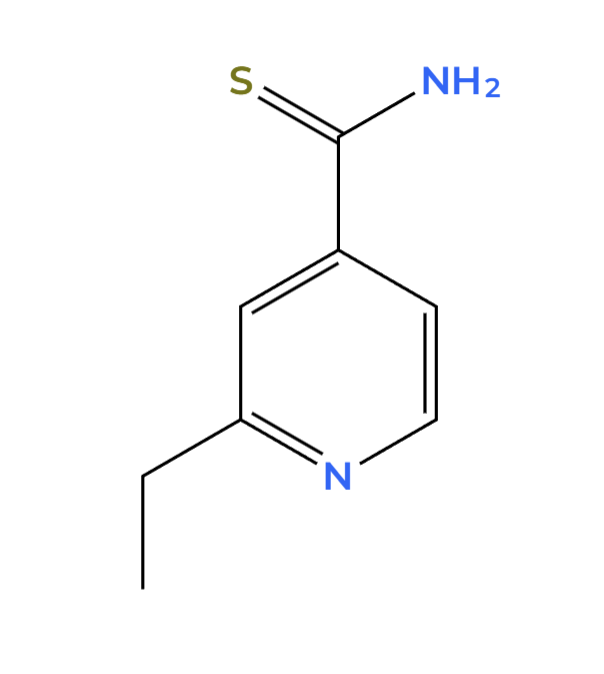
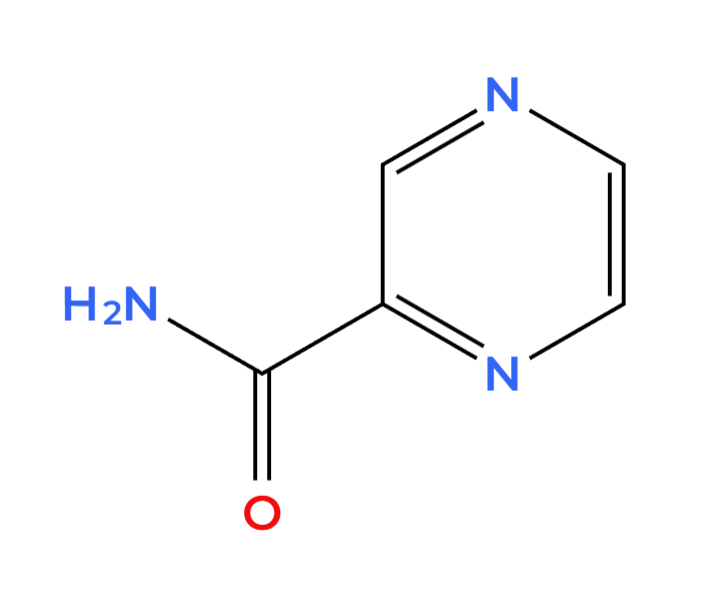
Chemical Structure and Molecular Formula of Ethionamide
Ethionamide is part of a group of compounds known as thioamides. It has a structure that includes a pyridine ring, with a thiocarbonyl functional group attached to it which is crucial for its antimicrobial effects, against Mycobacterium species.
Available Formulations (Tablets, Capsules, Liquid Formulations)
- Tablets come in oral form and are offered in various doses like 250 mg.
- For individuals experiencing sensitivity capsules offer a form of medication delivery tailored to their needs.
- Liquid suspensions are mainly used for children or individuals, with swallowing difficulties who need dosage adjustments.
Excipient and Inactive Ingredients in Commercial Preparations
Ethide formulations consist of a variety of ingredients that improve their stability. How well they are absorbed by the body.
- Microcrystalline Cellulose boosts the bonding and strength of tablets.
- Lactose Monohydrate serves as a filler to help distribute the medication.
- Magnesium Stearate acts as a lubricant to avoid tablet sticking while being produced.
- Facilitates the dissolution and disintegration of tablets to improve absorption efficiency is enhanced by Povidone.
How Ethide (Ethionamide) Works
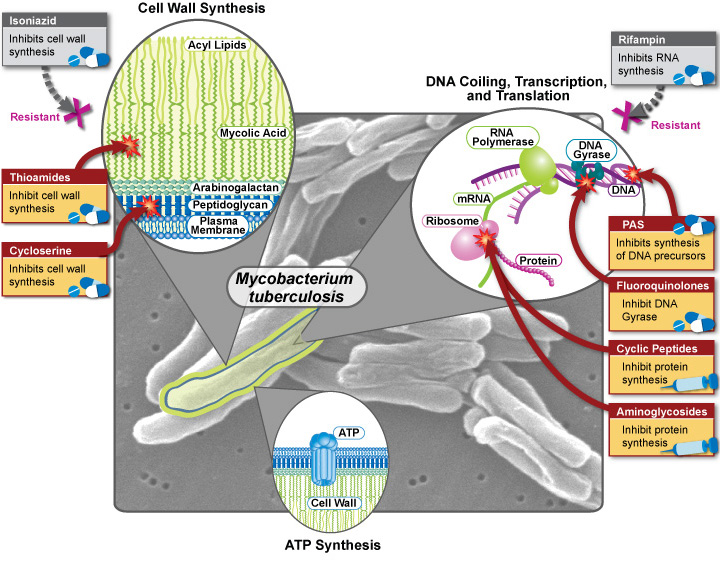
Mechanism of Action Against Mycobacterium Tuberculosis
Upon entering the body system Ethionamide goes through a process of activation, with the help of an enzyme called EthA producing active substances that block InhA an important enzyme involved in the production of mycolic acid. This blockage results in the formation of the cell wall causing an increase, in permeability and eventually leading to the death of bacteria.
Inhibition of Mycolic Acid Synthesis and Bacterial Cell Wall Disruption
Mycolic acids play a role in the strength and ability of Mycobacterium tuberculosis to cause disease in the body. Ethambutol interrupts their production process, it weakens the protective cell wall of the bacteria. This combined treatment has an impact, in killing the bacteria and treating tuberculosis effectively.
Comparison with Other Anti-Tuberculosis Drugs
- Both Isoniazid and Ethionamide work, in a way; however Ethionamide is considered as an alternative when resistance, to the develops.
- The main function of rifampicin is to block RNA production while ethionamide focuses on creating lipids in the body.
- Pyrazinamide works well in acidic environments while Ethionamide needs enzymes to become active.
- Bedaquiline: Disrupts ATP synthesis rather than cell wall integrity, making it mechanistically distinct.
Pharmacokinetics: Absorption, Metabolism, Half-Life, and Excretion
Ethionamide has absorption when taken orally and reaches its concentration, in the blood within two to three hours after ingestion. It undergoes metabolic transformation in the liver by flavin-containing monooxygenases into both active and inactive forms. The drug stays in the body for about 2 to 3 hours on average, which means it needs to be taken times a day for effectiveness. It is mainly eliminated through the kidneys and feces so extra care is needed when treating patients with liver issues.
Approved Uses of Ethide (Ethionamide)
Treatment of Multidrug-Resistant Tuberculosis (MDR-TB)
Ethide (also known as Ethionamide) plays a role, in tackling multidrug-resistant tuberculosis (MDR-TB) a significant public health issue marked by resistance to common antitubercular medications like rifampicin and isoniazid. As an option Ethionamide steps in when traditional treatments fall short by effectively killing bacteria through blocking the synthesis of mycolic acid, a key element in the mycobacterial cell wall. Managing MDR TB requires an approach involving medications due, to its challenging nature. Ethionamide is quite effective, in combatting Mycobacterium tuberculosis as it interferes with the bacterium's structure and limits its growth rate successfully. Despite its impact in treating the disease the use of Ethionamide is sometimes limited due, to the possibility of reactions, which requires careful monitoring during treatment.
Combination Therapy with Other Antitubercular Drugs
Treatment, with Ethionamide alone is not enough because bacteria quickly become resistant to it. Of using only Ethionamide treatment, for MDR-TB patients Doctors combine it with other second-line drugs to make the treatment more effective and reduce the chances of resistance emerging. Some of the drugs often used together with Ethionamide are;
- Levofloxacin and Moxifloxacin are types of antibiotics known as fluoroquinolones that work by blocking DNA gyrase to stop bacteria from reproducing.
- Cycloserine is an antibiotic that works by inhibiting the synthesis of cell walls.
- Capreomycin is an injectable aminoglycoside known for its ability to kill mycobacteria effectively.
- Linezolid is an antibiotic, in the oxazolidinone class that disrupts the synthesis of proteins.
Multidrug treatments boost the effectiveness of Ethambutol, in killing bacteria and improving treatment success rates by reducing their viability. It is crucial to follow combined therapy guidelines to avoid treatment failure and the development of resistance, in bacteria.
Treatment Duration and Effectiveness
The length of treatment, with Ethambutol depends on how serious the infection is how the patient responds to it well as the resistance patterns present. In general the standard treatment for multidrug tuberculosis lasts between 18 to 24 months. Ethambutol plays a crucial role in both the initial and maintenance phases. Attempts to assess its effectiveness involve examining radiological data. Regular sputum tests,chest scans and observation of symptoms are performed to evaluate the success of the treatment. Certain key factors affect how well the treatment works, such, as;
- Drug susceptibility is crucial, in determining the effectiveness of treatments, for M.tuberculosis based on its resistance profile.
- Patient cooperation is crucial as following the advised treatment plan is directly linked to eliminating the issue at hand.
- Managing Adverse Effects; Improving the management of side effects like stomach discomfort and nerve-related issues enhances how well people can tolerate and stick to their treatment plan.
Although Ethionaide is quite effective, in treating drug tuberculosis (MDR-TB) its usage is frequently restricted due to the potential for causing stomach issues and liver damage as well as affecting mental health negatively. Nonetheless, its significance in fighting against MDR TB is crucial, in instances where resistance patterns are widespread.

Off-Label Uses of Ethide (Ethionamide)
Treatment of Leprosy (Mycobacterium leprae)
Ethide (Ethionamide) has shown effects, beyond its main use in treating tuberculosis; it has also been studied as an additional treatment for leprosy on certain occasions – a persistent infectious condition caused by Mycobacterium leprae. While not commonly used as a first-choice medication for leprosy treatment due to its similarities with thioamide-based drugs like prothionamide Ethionamide potential role is being considered in cases where resistance, to multidrug therapy, is observed. The treatment of leprosy usually involves a combination of drugs;

- Rifampicin: A bactericidal agent that inhibits bacterial RNA synthesis.
- Clofazimine is a medication that helps reduce inflammation and fights, against types of bacteria by disrupting their cell membranes.
- The use of dapsone is essential, for managing leprosy as it acts as an inhibitor of synthase, in the body.
For individuals dealing with lasting or medication leprosy conditions Ethiomide has been considered as a possible substitute option, especially in instances where there is resistance, to rifampicin. Nevertheless, the side effects associated with it such, as liver toxicity and digestive system discomfort usually require the selection and monitoring of patients.
Potential Use in Non-Tuberculous Mycobacterial Infections
Non-Tuberculous mycobacteria (NTM) consist of various opportunistic pathogens, like Mycobacterium avium complex (MAC) Mycobacterium abscessus, and Mycobacterium kansasii that can lead to different types of infections affecting the lungs and skin as well as spreading throughout the body. Especially in people with weakened immune systems. Even though Ethioamide is not commonly prescribed for NTM infections tentative research shows it might be effective, against strains of the bacteria. Here are some important points to consider;
- When ethambutol is used together with macrolides (such, as clarithromycin and azithromycin) and aminoglycosides like amikacin can result in increased effectiveness, against bacteria.
- Targetting mycobacteria could be beneficial, in the treatment of disseminated NTM infections due, to its ability to penetrate cells effectively.
- Variable Sensitivity Levels ; Various types of NTM display varying reactions, to Ethionamide that require susceptibility assessments.
While these advantages are promising to consider the widespread use is hindered by the lack of data; more research is needed to better understand its specific impact, on NTM treatment.
Investigational Use in Buruli Ulcer Treatment
Buruli ulcer results from the presence of Mycobacterium ulcerans and manifests, as a skin and soft tissue infection marked by ulcerations that destroy tissue and cause illness. Standard treatment typically involves using both rifampicin and clarithromycin; difficult cases may require exploring treatment approaches. Researchers have looked into how Ethiomide disrupts the synthesis of acid and its potential effectiveness against M.ulcerans. Experimental studies done in labs and animal models have investigated its usefulness as a treatment, in resistant cases. Some potential benefits include;
- Tissue Penetration Effectiveness Boost; Ethionamide could potentially improve the effectiveness of antibiotics, in areas, with less blood supply.
- When used together Rifampicin and another medication can enhance their ability to kill bacteria effectively.
- Minimizing the Surgical Procedure Impact; Should the medication prove successful in treatment it could potentially lessen the requirement, for tissue removal.

Current studies are focused on finding the ways to use it in treating Buruli ulcers taking into account the doses and ensuring it is safe, for patients.
Experimental Applications in Drug-Resistant Bacterial Infections
The increasing worldwide challenge of resistance requires us to explore using medications to fight new types of harmful bacteria that are becoming resistant, to drugs. Ethionamide has primarily been used for treating tuberculosis. Is now being looked at for its ability to tackle drug-resistant bacterial infections. Key research areas include;
- Studies indicate that there might be some effectiveness, in combating methicillin-resistant Staphylococcus aureus (MRSA) as it can interfere with the synthesis of the cell wall, in Staphylococcus aureus infections.
- Preliminary studies are investigating the potential of Ethionamide, as a treatment, for resistant Gram-negative bacteria, specifically Carbapenem resistant Acinetobacter baumannii strains.
- Mycobacterial Co-Infections are currently being considered for inclusion, in treatment plans that target infections, which involve both tuberculosis and other opportunistic bacterial species.
Though these apps show promise and are still, in the stages they need thorough testing and validation, in clinical settings before being included in regular antimicrobial procedures.
Dosage and Administration Guidelines
Standard Adult Dosage for Tuberculosis Treatment
Ethide (Ethionamide) is a medication taken by mouth that is tailored to each patient based on their tolerance and response. The treatment dosage requirements vary between 500 mg and 1 g per day in adults being treated for tuberculosis it is usually split into two or more doses to make it easier on the stomach starting with a dose like 250 mg, per day and then slowly increasing to lessen any negative side effects during treatment commencement. In treating multidrug tuberculosis (MDR TB) Ethionamide plays a role, in second-line treatment plans and is commonly paired with other antitubercular medications such as fluoroquinolones and cycloserine or linezolid for effective results, through combined therapy supervision to ensure proper adherence and improve treatment effectiveness.
Pediatric Dosage Recommendations
The amount of Ethiomide given to children depends on their weight. Is calculated to ensure they get enough of the drug without risking side effects or toxicity issues.
Kids are usually prescribed, between 15 to 20 milligrams per kilogram per day. They take this in two or more doses throughout the day. Doctors usually don't give children more than milligrams a day.
Children might feel the side effects of Ethiomide more strongly than adults like stomach problems and issues with their nerves. Because of this doctors often start with doses. Increase them slowly over time.
Sometimes doctors may also monitor how much of the drug is, in a child's system if they need to take Ethiomide for a longtime.

Dose Adjustments for Renal and Hepatic Impairment
Ethionamide is mainly broken down in the liver. Should be used carefully in patients, with liver issues. It is recommended to conduct baseline liver function tests for those, with existing liver conditions and continue monitoring their liver function over time. If liver enzyme levels rise significantly – three times above normal with symptoms or five times without – reducing the dosage or stopping the medication may be necessary. Ethionamide clearance is not greatly affected by kidney problems because it is primarily eliminated through liver metabolism. Henceforth no changes, in dosage are typically needed for mild to kidney issues; nevertheless it's advisable to be careful, with patients facing kidney problems or using drugs that may harm the kidneys concurrently.
Administration with or Without Food Considerations
Ethionamide can be taken with or, without food. Having it with meals could help reduce stomach issues like nausea and feeling uncomfortable in the abdomen area known as epigastric discomfort." It might be easier on the body, with foods involved for drug tolerance. Key points to remember when taking it;
- During meals can help reduce stomach discomfort and improve compliance, with the medication regimen.
- Fasting may help with absorption. This could lead to stomach issues.
- Steer clear of alcohol to reduce the chances of liver damage and worsening issues.
Recommended Duration of Therapy and Adherence Importance
The length of Ethambutol treatment varies based on the reason, for use and how susceptible the bacteria is to it. While treating drug-resistant tuberculosis (MDR TB) the therapy typically extends for 18 to 24 months. It involves a phase lasting at least six months followed by a continuation stage. Following the regimen diligently is crucial as stopping or having doses raises the chances of treatment not working well and XDR TB developing. To ensure patients stick to their medication routine support strategies, like counseling and drug observed therapy (DOT) are utilized.
Common Side Effects of Ethide (Ethionamide)
Gastrointestinal Side Effects: Nausea, Vomiting, Diarrhea, Abdominal Pain
Ethiomide is known to cause some side effects, such as vomiting, nausea and stomach pains, for patients taking it regularly over time periods ranging from weeks, to months after starting the medication regimen. Methods to cope with stomach-related problems;
- Divided dosing refers to breaking up the dose into several smaller doses throughout the day.
- When taking food having it with meals can help lessen feelings of nausea.
- When dealing with cases consider recommending metoclopramide or ondansetron as nausea remedies.
Diarrhea and indigestions can also occur at times; they are usually temporary. Should be looked into if they persist or become severe. Improving hydration and making changes are crucial, for managing these symptoms.

Neurological Effects: Dizziness, Headache, Peripheral Neuropathy
Neurotoxic reactions such, as feeling lightheadedness and headaches and experiencing disruptions may arise at elevated dosages. The impact of Ethiomide on nerve cell operation could also lead to symptoms like tingling or numbness in the limbs. Recommended approaches, for prevention and treatment include;
- Taking Vitamin B5 (Pyridoxine); May reduce nerve damage risks during treatment periods.
- Adjustment of the dosage might help reduce symptoms in individuals who are more sensitive, to it.
- Close observation is crucial, for individuals, with existing nerve-related ailments or those taking medications simultaneously.
- Severe neurological symptoms, like psychosis or depression, are uncommon but they require medical attention.

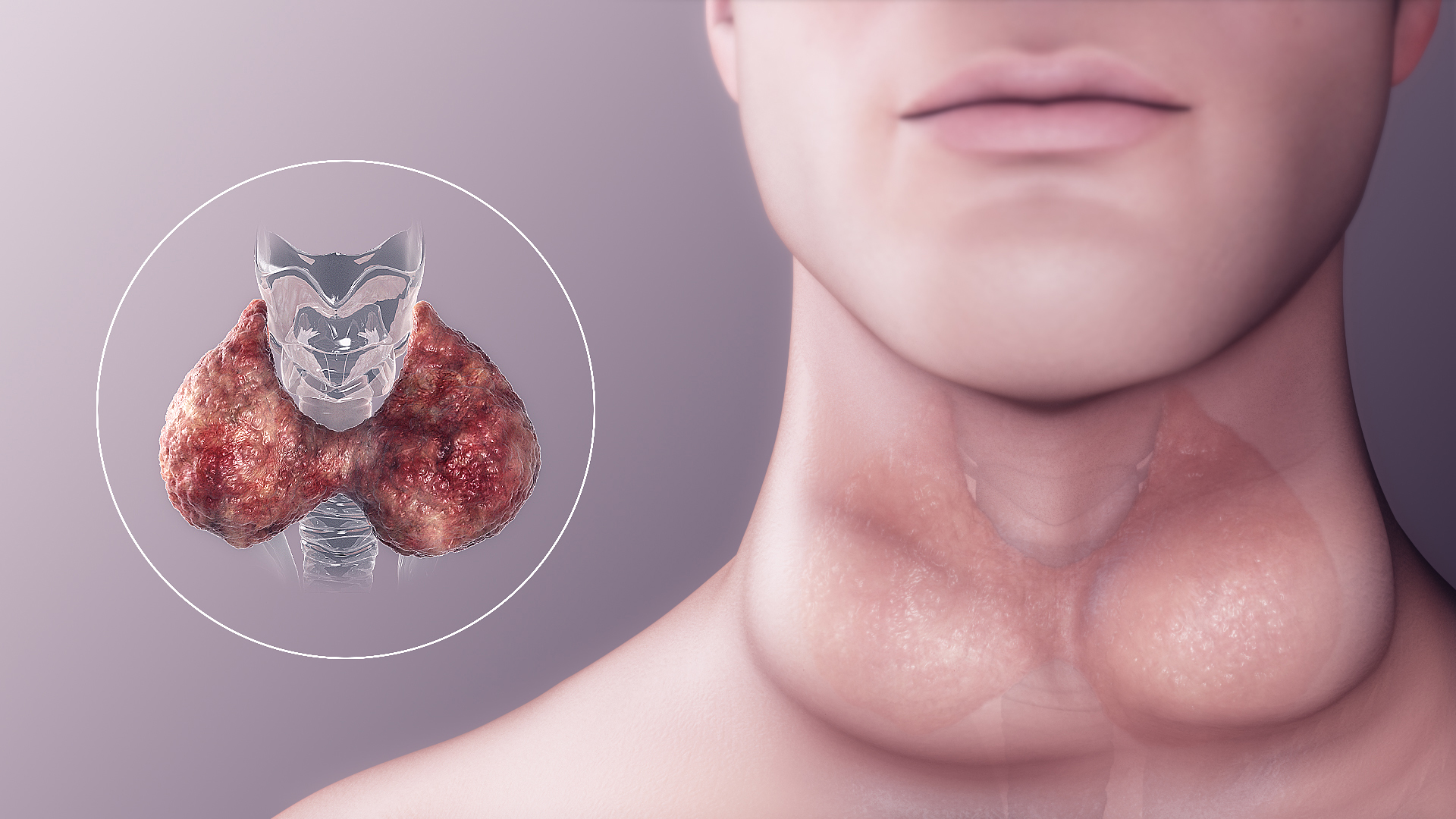
Endocrine Effects: Hypothyroidism and Its Management
Ethionamide has the capability to cause hypothyroidism when used alongside medications, like para-aminosalicylic acid (known as PAS). The reason, behind this occurrence is linked to the drugs hindrance to the production of thyroid hormones. Signs of hypothyroidism may include;
- Feeling lacking energy
- Putting on pounds
- Feeling sensitive, to temperatures.
- Feeling low in spirits.
Regular monitoring of thyroid function is advised for individuals, on long-term treatment regimens to detect any issues on in the process of recovery, from tuberculosis treatment if hypothyroidism is detected.
Dermatological Reactions: Rash and Photosensitivity
Some people may experience skin reactions to Ethioamide that can vary from rashes, to serious hypersensitivity reactions. Though rare photosensitivity reactions require steps, like applying broad-spectrum sunscreens and wearing clothing.When it comes to handling side effects;
- Antihistamines can help reduce itching or redness in reactions, on the skin.
- Topical corticosteroids are effective, for treating areas of inflammation in the body.
- In situations where there are severe allergic reactions, Stevens-Johnson syndrome can occur therefore drug use has to be discontinued
Serious Side Effects and Adverse Reactions
Hepatotoxicity and Liver Enzyme Elevation
Ethide (Ethionamide) is extensively metabolized in the liver which makes the liver vulnerable, to its effects such as transaminases and cholestasis leading to severe conditions, like fulminant hepatic failure. The factors that increase the risk of Ethionamide-induced liver damage are well documented.
- Patients who already have liver conditions, like hepatitis or cirrhosis face an increased risk factor.

- Hepatotoxic drugs that are taken together with other drugs, like Isoniazid or Rifampin can worsen liver strain and pose a risk to liver health.
- Drinking alcohol can increase liver enzyme levels and cause damage, to liver cells.
Before starting treatment, for any condition or illness that requires medication initiation Liver Function Tests (also known as LFT tests for short) should be conducted as a baseline measurement of liver health and functions to ensure safety and effectiveness during the treatment process. Throughout the treatment regimen it is essential to monitor liver function to assess any changes or abnormalities that may occur to adjust dosage or consider discontinuation if necessary.
If levels of transaminases in the liver exceed three times the limit accompanied by symptoms or rise up to five times without any noticeable symptoms it is advisable to evaluate the situation for potential discontinuation of medication or modification in dosage, as a precautionary measure.
Neurotoxicity and Psychiatric Effects (Depression, Confusion, Psychosis)
Neurotoxicity poses a risk when undergoing Ethionamide treatment and can lead to issues such as cognitive impairment or mood changes along with peripheral neuropathy symptoms, like central nervous system (CMS).
- Patients experiencing depression and thoughts of suicide may show disinterest in things they used to enjoy or display self-behaviors.
- In instances of health conditions such, as psychosis arise symptoms, like hallucinations and paranoia have been documented.
- Symptoms of impairment may include confusion and difficulties, with memory and focus.
Peripheral neuropathy is a condition known for causing tingling sensations and muscle weakness due, to Ethionamide affecting nerve function.Vitamin B6 supplementation is advised to lessen nerve related issues in individuals undergoing treatment.
If severe neuropsychiatric side effects occur, dosage adjustment or stopping treatment may be necessary along with support, for symptoms.
Severe Gastrointestinal Disturbances and Malabsorption
Experiencing stomach discomfort is usual; however if the issues become severe it could greatly impact a patients ability to follow their treatment regimen effectively and consistently over time.

- Severe diarrhea may lead to difficulty, in absorbing nutrients essential for the body's function.
- Symptoms of irritation can include pain, in the abdomen (epigastric pain) indigestion (dyspepsia) or even the development of stomach ulcers.
Persistent digestive issues might require treating the symptoms with medications, like nausea drugs (such as ondansetron and metoclopramide) or acid-reducing drugs like omeprazole and pantoprazole when necessary, for relief.
Hematologic Abnormalities: Anemia, Leukopenia
Ethionamide may cause blood-related issues, in patients who undergo long-term treatment with it and could lead to abnormalities such, as;
- Anemia is commonly characterized by red blood cells and normal levels of hemoglobin, in the blood due, to bone marrow suppression.
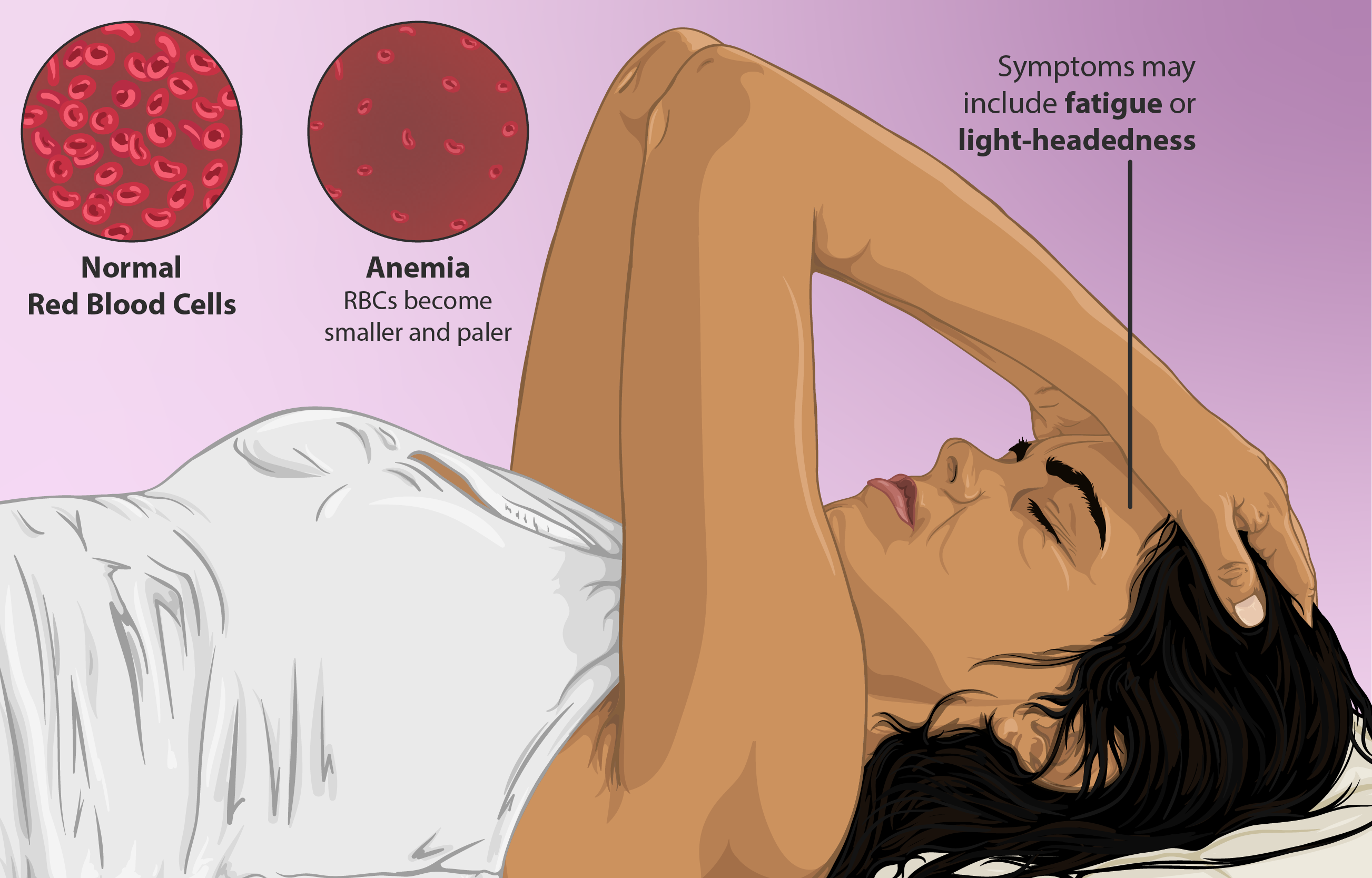
- Leukocytosis refers to a decrease, in the number of blood cells in the body which can make patients more susceptible, to infections.
- Thrombocytopenia is uncommon. Could be serious as it raises the chances of bleeding issues occurring.
Regular blood tests are suggested to monitor blood counts and treatment may be stopped if there are decreases, in cell counts such, as due to anemia or low platelet counts or transfusions might be required in cases of severe bone marrow suppression.
Drug Interactions with Ethide (Ethionamide)
Interaction with Other Anti-Tuberculosis Drugs (Isoniazid, Rifampin, Pyrazinamide)
Ethionamide is frequently used in combination with other anti-tubercular agents, yet its co-administration necessitates careful monitoring due to potential pharmacokinetic and pharmacodynamic interactions.
- Isoniazid: Combined neurotoxic effects, increasing the risk of peripheral neuropathy and CNS disturbances.
- Rifampin: Potentiates hepatotoxicity, necessitating close monitoring of liver enzymes.
- Pyrazinamide: Exacerbates gastrointestinal intolerance and hepatotoxic effects.
Adjunctive pyridoxine supplementation is strongly recommended in regimens containing both Ethionamide and Isoniazid to mitigate neurotoxicity.
Potential Interactions with Antiepileptic Drugs (Phenytoin, Carbamazepine)
Ethionamide can impact the activity of liver enzymes. It may change how antiepileptic drugs are metabolized. Important interactions to watch out for in practice are;
- Phenytoin may lead to levels, in the blood which can raise the chances of experiencing toxicity symptoms, like unsteadiness (ataxia) eye movements (nystagmus), and confusion.

- Carbamazepine can lead to levels, in the bloodstream that may increase the risk of nervous system depression and liver damage.
Patients who are taking drugs at the same time need regular monitoring of their drug levels to prevent any harmful effects or insufficient efficacy of the medication they are receiving and sometimes adjustments, to the dosage may be needed to ensure that their seizures are well managed.
Effects on Diabetes Medications and Hypoglycemia Risk
Ethionamide can affect the balance of glucose, in the body and raise the chances of causing blood sugar as a side effect of the medication; this risk is especially heightened in individuals, with diabetes. The ways in which this happens are as follows;
- Stimulating beta cells increases insulin release and reduce blood sugar levels.
- Inhibiting hepatic gluconeogenesis helps decrease the body's production of glucose.
Patients who are taking medications, like sulfonylureas (such as glibenclamide or gliclazide) or insulin treatments should regularly check their blood sugar levels. In case of hypoglycemia occurrences adjustments, to the dosage of diabetes medication and dietary changes may be needed.
Contraindications with Alcohol and Hepatotoxic Agents
Ethionamide demonstrates a reaction when consumed with alcohol that results in an antabuse response featuring;
- Redness, in the face and blushing.
- Tachycardia and palpitations
- Experiencing feelings of nausea and vomiting
- Feeling lightheaded and experiencing high blood pressure
Furthermore Drinking alcohol greatly increases the effects Ethinamide can have on the liver and requires avoidance of it. Using substances that are harmful, to the liver like acetaminophen or certain medications along, with Ethinamide can raise the risk of liver damage even more. Patients need to be informed about the importance of steering of alcohol and other substances that harm the liver to reduce effects and improve treatment results.

Contraindications and When Not to Use Ethide (Ethionamide)
Absolute Contraindications: Severe Liver Disease, Hypersensitivity Reactions
Ethide (Ethionamide) should not be used by individuals, with liver problems because it is extensively metabolized in the liver and can potentially cause liver damage. People with conditions like cirrhosis or acute hepatitis have a chance of drug-induced liver injury that could lead to liver failure. Another absolute reason not to use Ethide is if someone has shown a reaction to Ethionamide or similar substances, in the past.
- Severe skin reactions such, as hives (urticaria) swelling (angioedema) or Stevens-Johnson syndrome can occur.
- Anaphylaxis is a condition that can be life-threatening marked by difficulty breathing and unstable blood pressure.
People who have had reactions, to Ethionamide or similar thioamides should completely steer clear of using it again because it might trigger a serious immune related reaction upon re-exposure.
Pre-Existing Psychiatric Disorders and Neurological Conditions
Ethionamide has been found to have effects, on the system and is not recommended for those, with preexisting psychiatric or neurological disorders as it can worsen their condition by;
- Feeling down and struggling with mood swings can lead to thoughts of self-harm and emotional volatility for those dealing with depression or mood disorders.
- Experiencing psychosis can worsen symptoms of schizophrenia. Result from drug-induced hallucinations.
- Potential decrease, in seizure threshold, may occur in individuals, with epilepsy and seizure disorders.
Before starting any treatment involving Ethionamide in patients, with a mental health background history of mental illness assessments need to be conducted carefully to ensure safety and effectiveness throughout the therapy process It is crucial to monitor closely for any neuropsychiatric side effects and make necessary dose accommodations or consider other treatment options if symptoms show signs of aggravation.
Pregnancy and Risk of Fetal Harm
Ethionamide falls under pregnancy category C which indicates harm to the fetus according to animal research findings Limited human studies also hint at a chance of birth defects especially if taken in the initial trimester Potential risks to the unborn baby may include;
- Potential developmental delays may occur as a result of impairment stemming from effects.
- The limitation of growth, in a fetus is linked to extended exposure, within the womb.
It is recommended that pregnant individuals steer clear of using ethionamide unless the advantages outweigh the risks involved— in situations, like multidrug tuberculosis where safer alternatives are scarce. For women capable of bearing children receiving treatment with ethionamide should consider contraception as a measure.
Important Precautions Before Taking Ethide (Ethionamide)
Regular Liver Function Monitoring and Hepatic Safety Precautions
To ensure safety during treatment, with Ethambutol due to its liver effects factor, liver function tests before and during therapy to monitor for any signs of liver damage or abnormal levels that require prompt review and adjustment of treatment plans. These measures help reduce risks to the liver health;
- Remember to keep an eye, on ALT and AST levels, as total bilirubin every four to six weeks when undergoing long-term treatment.
- Try to steer off taking medications that could harm your liver alongside ones, like Isoniazid (INH) Rifampin (RIF) and Pyrazinamide (PZA) if you can help it.
- If serious liver damage is detected it is advisable to stop the treatment particularly when liver enzyme levels exceed five times the limit of range.
If someone shows signs, like yellowing skin or eyes (jaundice) dark urine coloration, feeling of sickness (nausea) or tiredness without a clear reason (fatigue) it's important for them to get their liver checked quickly to make sure it's not because of medication harming the liver.

Blood Glucose Monitoring for Diabetes Patients
Ethambutol disrupts the process of glucose breakdown, in the body. Can raise the chances of blood sugar in individuals with diabetes by affecting insulin release and blocking liver glucose production. Don't forget that patients with diabetes should always be cautious, about this risk.
- Be sure to check your blood sugar levels especially when starting a treatment or making changes, to your diabetes medications.
- Make changes, to the dosage of diabetes medications or insulin to avoid experiencing blood sugar symptoms.
- Identifying the signs of hypoglycemia includes symptoms such, as sweating, heart palpitations feeling dizzy, and experiencing confusion.
It is recommended for individuals, with diabetes who are taking Ethionamide to have check-ups with an endocrinologist to maintain blood sugar levels during the treatment period.
Avoidance of Alcohol and Hepatotoxic Drugs
When taking Ethionamide medication it is important to avoid alcohol as it can cause reactions, like flushing, tachycardia, nausea and vomiting similar to Antabuse effect and worsen liver damage in those at risk for liver problems.
It is also advisable to limit the use of substances that may harm the liver such, as acetaminophen and certain antifungal drugs while on Ethionamide treatment to lower the chances of liver damage accumulation.
Importance of Vitamin B6 Supplementation to Prevent Neuropathy
Ethionamide is known to impact neuropathy by disrupting pathways that rely on pyridoxine and causing nerve dysfunction symptoms such, as;
- Feeling of pins and needles. Tingling in the arms and legs.
- Experiencing a sensation of burning or heightened sensitivity to touch.
- The inability to sense body position and control movements effectively leading to challenges, in the coordination of motor skills.
To address nerve-related issues effectively and protect against problems caused by Vitamin B deficiencies, in the body's system supplementing with Vitamin B (Pyridoxine) at a daily dosage of 50 to 100 mg is commonly advised. This dose not aids in averting nerve damage but also boosts the functioning of the nervous system. For those already experiencing symptoms a higher intake may be required along, with nerve function evaluations to gauge the effectiveness of the treatment plan.
Special Considerations for Specific Populations
Administration to Elderly Patients
Increased Risk of Hepatotoxicity and Neurotoxicity
Ethide (Ethionamide) must be administered cautiously to individuals because their bodies undergo changes as they age that impact how the drug is metabolized and eliminated from the system. Elderly people are, at a risk of experiencing liver damage due to a decrease in liver enzyme efficiency as they get older. This makes them more prone to liver issues caused by medication that can lead to symptoms such as yellowish skin coloring (jaundice) tiredness (fatigue) and increased levels of enzymes in the blood. Moreover older patients are more vulnerable to nerve and brain-related side effects like nerve damage, in the limbs ( neuropathy) and cognitive decline. Symptoms, like feeling lightheadedness or confusion and tingling sensations can make it hard to move around and raise the chances of falling henceforth requiring observation.

Dose Adjustments Based on Renal and Hepatic Function
Even though Ethionamide is mainly processed by the liver changes may occur in how it works in patients, with liver or kidney issues. It's important to think about adjusting the dosage in these situations;
- In case of liver issues and elevated enzyme levels, in liver function tests occur it may be necessary to adjust the dosage or the timing, between administrations.
- Renal issues should be monitored in patients, with kidney problems even though Ethionamide is mostly eliminated through renal pathways to avoid potential toxicity buildup when combined with other drugs that may harm the kidneys.
It's crucial to monitor individuals, under clinical care to reduce negative effects and ensure the best possible treatment outcomes.
Monitoring for Cognitive and Metabolic Changes
As people age and undergo Ethiomide treatment might experience issues, like memory loss and feeling confused or sad similar to dementia or Parkinson's disease symptoms. Furthermore the drug can affect glucose levels so it's important to watch for blood sugar, in older patients with diabetes. If someone suddenly feels disoriented or agitated it could be a sign of a blood sugar drop.
Administration to Pregnant Women and Nursing Mothers
Pregnancy Category and Potential Teratogenic Risks
Ethionamide falls under the Pregnancy Category C drug classification due, to findings from animal studies showing harm to fetuses; however limited human data is available, on this issue. Risks linked to Ethionamide exposure during pregnancy involve effects.
- In studies, with animals, researchers have noted abnormalities in the structure of the face and skull in relation, to the mouth and facial features.
- Concerns, about the impact of neurotoxicity, in fetuses include delays and neurological deficits.
- Prolonged use, by the mother could possibly hinder the growth of the fetus.
Ethionamide could potentially be an option, for treating multidrug-resistant tuberculosis (MDR-TB) especially when other treatment options are scarce or inadequate despite the risks.

Risk-Benefit Analysis in MDR-TB Cases During Pregnancy
Expecting mothers who have multidrug tuberculosis face the challenge of balancing their well-being with the safety of their unborn baby's health. There are heightened risks associated with TB for both the mother and the child such, as birth, a low birth weight and a higher chance of infant mortality. When Ethionamide is necessary, for treatment certain precautions need to be followed;
- Infectious disease specialists and obstetricians working together in consultations to decide on the treatment approach.
- Routine checks, on development involve ultrasounds and assessments to identify any possible developmental issues early on.
- It is recommended to take Vitamin B5 (Pyridoxine ) to lessen the effects, on the nerves.
When there are options it might be a good idea to replace Ethionamide with different second-line medications.
Breastfeeding Safety and Lactation Concerns
The safety of Ethionamide while breastfeeding is still unclear because there is no data, on how it passes into breast milk.
- The impact of neurotoxicity, on babies may manifest as decreased muscle tone (hypotonia) fussiness (irritability), or challenges with feeding.

- Changes, in liver function in infants may occur because of the risk of the drug building up, in their system.
If there isn't safety information available yet, about breastfeeding while taking Ethiomide medication it's important for nursing mothers to talk to their doctor about the potential risks and benefits involved in order to make an informed decision. It is advisable for healthcare professionals to closely observe the baby for any reactions if Ethiomide treatment is unavoidable, in cases.
Administration to Children and Adolescents
Approved Pediatric Dosing and Safety Considerations
Ethionamide has been given the light, for treating children with drug tuberculosis specifically. The prescribed dosage schedule is as follows;
- 15 to 20 milligrams, per kilogram, per day should be split into two or more doses throughout the day.
- The recommended highest amount, for daily intake is 1 gram.
In order to account for differences, in how drugs are processed in the body of children it is important to tailor the dosage based on each child's needs to ensure that the treatment is effective and well tolerated. It is also crucial to take into account the history of children, with liver or brain conditions.
Neurological and Gastrointestinal Side Effect Risks
Kids are particularly sensitive, to the digestive impacts of Ethionaide, with common side effects often seen in young patients including;
- Feeling dizzy and tired can make it hard to do well in school.
- Symptoms of neuropathy may include weakness or a sensation of numbness or tingling in the limbs.
- Severe nausea and vomiting can lead to a decreased appetite. Resulting in weight loss.
Supplemental intake of Vitamin B6(Pyridoxine), in children is essential to reduce the risk of issues.

Alternative Treatment Options for Pediatric Tuberculosis
When children cannot handle Ethionamide well due, to side effects or intolerance issues in treating tuberculosis infection. Doctors may need to explore options for second-line medications that are better suited, for them. Some alternatives to consider include;
- Levofloxacin or Moxifloxacin are fluoroquinolones that have a range of effectiveness, against drug-resistant tuberculosis strains.
- Cycloserine is a type of medication that can help fight against strains of bacteria that are resistant, to treatments.
- Linezolid is a type of antibiotic known as oxazolidinone that is utilized to treat cases of multidrug tuberculosis (MDR TB).
Treatment decisions should depend on the results of drug resistance tests, such as how well the patient can tolerate the medication and how they respond to it clinically.
Handling Precautions and Safe Storage
Proper Handling and Disposal of Ethionamide Tablets
- Proper care is essential when dealing with ethiomamide to safeguard patients and avoid exposure risks. It is important to handle this drug with clean and dry hands to prevent moisture-related degradation. Crushing or splitting the tablets should be avoided unless a healthcare provider advises otherwise as altering the form could affect how the drug is absorbed and its effectiveness. To prevent harm and accidental ingestion of unused or expired ethiomamide it's critical to dispose of it. Guidelines for disposal include;
- Pharmaceutical disposal programs are considered the safest and most environmentally friendly choice available.
- If there's no program, take the medication you're done with and dispose of it without risk to others or the environment. You can mix it with coffee grounds or cat litter before throwing it in a secure container.
To protect the environment and prevent water pollution please do not dispose of ethionamide by flushing it down the toilet unless instructed to do so by a professional.
Storage Conditions: Temperature, Moisture, and Light Sensitivity
Ethionamide is prone, to breaking down in the environment. Should be kept in conditions to preserve its effectiveness, as a medical product.
- Remember to keep the product within a temperature range of 15°C to 25°C (59°F to 77°F) making sure to avoid exposing it to cold conditions.
- Remember to store it in a place to avoid moisture damage; stay clear of settings, like bathrooms or kitchens.
- Remember to keep the product from sunlight and UV exposure by storing it in a container that shields against light sensitivity.
Failure to follow these storage instructions could lead to the deterioration of chemicals, in the medication or a decrease in effectiveness and potentially an elevated possibility of side effects due to changes, in the drugs composition.
Keeping Medications Out of Reach of Children and Pets
Ethiomide can be harmful if ingested by children or pets accidentally due, to its effects, on the nervous system and liver; thus caution is required to avoid any mishaps.
- Make sure to store the medication in a cupboard or somewhere hidden and not easily accessible.
- Make use of prescription bottles with childproof caps to reduce the risk of ingestion by children.
- In the event of ingestion promptly seek emergency help or contact a poison control center.
Making sure to store medications is essential, for safeguarding those who are at risk and for maintaining the effectiveness of the medication, in treating conditions.

Overdosage and Toxicity Management
Symptoms of Ethionamide Overdose: Severe Vomiting, Seizures, Metabolic Acidosis
An overdose of Ethambutol can trigger a series of symptoms that pose a threat, to life by impacting the nervous system (brain and spinal cord) digestive system (stomach and intestines), and the body's metabolic processes.
- Experiencing stomach troubles, like queasiness throwing up, and intense stomach pains can be quite uncomfortable.
- Neurological toxicity can manifest as seizure changes, in state feelings of dizziness, and lapses, in consciousness.
- Metabolic acidosis can result from acidosis or hyperventilation. This may lead to electrolyte imbalances caused by disruptions, in metabolic functions.
In situations of overdose toxicity that is left untreated can lead to organ failure and may require intensive medical care.
Emergency Treatment and Supportive Care
Prompt medical care is crucial, in cases of suspected Ethionamide overdose, with actions including;
- Make sure the airway is clear and provide oxygen if there are breathing difficulties.
- Ensure hydration and balance of electrolytes by administering fluids as needed.
- In case of seizures use benzodiazepines such, as lorazepam or diazepam, for control.
- Correcting metabolic acidosis may necessitate the use of intravenous sodium bicarbonate to rebalance the body's acid-base levels.
In cases of overdose, it is advisable to hospitalize the individual and ensure cardiac monitoring to avoid potential issues, like irregular heartbeats or difficulty, in controlling seizures.
Role of Activated Charcoal and Symptomatic Management
Activated charcoal plays a role, in treating overdoses when given after ingestion. Ideally within one to two hours. Through adsorption in the tract it hinders the absorption of Ethionamide. Other approaches, for managing symptoms include;
- Medications such, as Ondansetron or promethazine are used to help manage vomiting episodes.
- Replacement of electrolytes may be necessary if test results show levels of potassium and magnesium in which case supplementation is recommended.
In some instances hemodialysis may be considered if severe metabolic imbalances continue despite therapies.

Monitoring for Long-Term Effects of Overdose
It is crucial to conduct follow-up monitoring after treatment to identify any lasting impacts of Ethionamide toxicity as there may be long-term issues that could arise.
- Persistent cognitive impairment or neuropathy can result from sequelae.
- Liver issues may occur over time. Will need monitoring to check how well the liver is functioning.
- Chronic gastrointestinal issues, like nausea or difficulty with absorbing nutrients may occur due to dysregulation, in the system.
Consistently checking in with healthcare helps address any remaining impacts promptly and effectively.
Conclusion and Final Recommendations
Summary of Key Benefits and Risks of Ethide (Ethionamide)
Ethionamide continues to play a role, in treating multidrug-resistant tuberculosis (MDR-TB) by effectively targeting resistant strains of mycobacteria and killing them off. Its importance, in the treatment of tuberculosis cannot be overstated; however, its use requires an evaluation of the risks and benefits involved. Key advantages;
- Works well against Mycobacterium tuberculosis strains that are resistant, to drugs.
- Important, in the treatment of tuberculosis when the initial therapy is not effective.
- Taking medication orally makes the treatment process easier, in comparison, to using injections.
Potential dangers to consider;
- There is a risk of liver and nerve damage.
- Significant digestive discomfort impacting the ability to stick to the treatment regimen.
Certain restrictions apply to, at risk groups such as mothers and people, with health conditions.
Adherence to Prescribed Dosage and Medical Supervision
Following the recommended dosing instructions is crucial to get the most out of treatment benefits and reduce the risk of developing resistance to medication .It is important for healthcare providers to closely monitor and modify treatment plans according to how patients are responding to the medication and their ability to tolerate it well as any relevant lab results .Patients are advised to;
- Remember to stick to a schedule, for taking your medication to ensure that the drug levels, in your body stay just right.
- Please make sure to report any reactions to avoid any further issues or complications.
- Make sure to have tests done at the lab to keep an eye on your liver health and check your blood sugar levels and brain function too.
When to Seek Medical Advice for Adverse Reactions
If patients encounter any of the following symptoms they should promptly seek assistance;
- Constant feelings of queasiness. Upset stomach, along, with yellowing skin (a sign of liver damage).
- Significant shifts, in mood and perception such, as hallucinations or confusion may indicate symptoms.
- Early signs of neuropathy may include a sensation of tingling or numbness, in the extremities.
- Experiencing hypoglycemia can lead to symptoms like feeling dizzy and sweaty with trembling sensations.
Ethide, Ethionamide FAQ
How does Ethionamide work
Ethionamide hinders the production of acid which is essential, for the structure of the cell wall in mycobacteria. It is designed as a prodrug that becomes active inside the cell and hampers the enzyme InhA. This action disrupts the integrity of the cell wall. Ultimately causes bacterial demise. Its impact, on bacteria can vary from inhibiting growth to causing death based on the concentration and vulnerability of the strain.
What is the drug Ethionamide used for?
Ethionamide is mainly employed in treating drug-resistant tuberculosis (MDR-TB). Additionally it might be recommended for leprosy in combined treatments when initial medications are ineffective or not recommended for use due, to contraindications playing a part, in WHO-supported second-line therapy guidelines.
Is Ethionamide a first line drug?
Ethionamide is not considered a medication, for tuberculosis treatment; it is categorized as an antitubercular treatment usually utilized when there is resistance to or inability to tolerate first-line medications, like Isoniazid or Rifampicin.
What is the difference between Ethionamide and Isoniazid?
Both Ethionamide and isoniazid prevent the production of acid in ways due, to their unique structures and activation processes. There is a variation, in how they're activated. Ethionamide needs the help of a flavin monooxygenase (EtaA) while Isoniazid relies on the catalase peroxidase enzyme (KatG). Moreover Ethionamide is known to cause system related side effects and is usually prescribed for cases where standard treatments are ineffective.
What is the mechanism of action of Ethionamide in leprosy?
In cases of leprosy treatment Ethionamide works by blocking the creation of acids, in Mycobacterium leprae which causes damage to the bacterias shell. It aims at the InhA enzyme just like it does in tuberculosis treatment interferes with the formation of the wall and results, in either slowing down or killing off the bacteria depending on its growth stage.
What is Ethionamide activated by?
Ethionamide gets activated by an enzyme called Etaa which is a flavin containing monooxygenase enzyme.This process changes the prodrug into a form that stops the Inha enzyme, from carrying out mycolic acid synthesis.
Is Ethionamide effective?
Ethionamide proves to be useful when included in combined treatments, for Multi drug Tuberculosis (MDR TB) and specific types of leprosy cases; its effectiveness relies on the vulnerability of bacteria and how well patients stick to the treatment plan; however adverse reactions may hinder its acceptance by some people.