Ranitidine Injection
- Introduction to Ranitidine Injection
- Composition of Ranitidine Injection
- Uses of Ranitidine Injection
- Off-Label Uses of Ranitidine Injection
- How Ranitidine Injection Works
- Dosage and Administration Guidelines
- Common Side Effects of Ranitidine Injection
- Detailed Analysis of Ranitidine Injection Side Effects
- Interactions with Other Medications
- Warnings and Contraindications
- Careful Administration of Ranitidine Injection
- Important Precautions with Ranitidine Injection
- Administration to Specific Populations
- Handling Overdosage of Ranitidine Injection
- Storage and Handling Precautions for Ranitidine Injection
- Conclusion: The Future of Ranitidine Injection in Medical Practice
Introduction to Ranitidine Injection
Ranitidine, a component of our pharmacological toolkit, represents the perfect blend of scientific innovation and medical necessity. This medication is widely recognized for its effectiveness in reducing stomach acid levels. Has gained popularity in both over-the-counter and prescription contexts. This discussion will focus on its form, which offers a unique approach to administering this potent H2 antagonist.
- One of the uses of Ranitidine is to protect against peptic ulcers, gastroesophageal reflux disease (GERD), and other conditions that cause discomfort or potential complications due to excessive stomach acid. It also plays a role in preoperative and intensive care units where controlling acid levels is essential.
- Modern medicine heavily relies on Ranitidine injections because they produce therapeutic effects and are highly versatile. The injectable form ensures relief, which becomes critical in acute care settings where oral administration may not be feasible or practical.
Composition of Ranitidine Injection
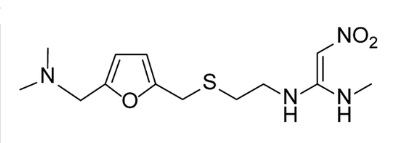
The creation of Ranitidine injection is a precise process in the field of pharmacology. It's more than turning the oral version into a liquid form:
- It's a meticulously calculated solution that ensures optimal effectiveness and safety when given through an IV or IM.
- At its core, the active ingredient remains Ranitidine hydrochloride, which selectively blocks histamine H2 receptors in parietal cells, thereby reducing gastric acid production.
- Stabilizers and solvents are included to maintain the compound's stability and solubility. Unlike Ranitidine, the injectable form doesn't have certain additives necessary for tablet formulation.
This difference affects how it works in the body and expands its usefulness as an option for patients who can't take medication orally or need immediate relief from excess stomach acid.
Uses of Ranitidine Injection
Ranitidine Injection is widely used due to its effectiveness in treating conditions caused by excessive stomach acid. It plays a role in the medical field, addressing common and complex gastrointestinal disorders.
- One of its uses is treating peptic ulcers, where it acts as a protective shield for the stomach lining against the damaging effects of acid. In cases of Gastroesophageal Reflux Disease (GERD), Ranitidine acts as a defense mechanism by reducing the backflow of acid into the esophagus. This helps alleviate symptoms and prevents damage to the esophagus.
- In addition to these uses, Ranitidine Injection is also helpful for managing Zollinger-Ellison Syndrome, a condition characterized by excessive gastric acid production.
- It is also used prophylactically to prevent stress-induced ulcers in critically ill patients. The versatility of Ranitidine highlights its role in modern gastroenterological treatments.
Off-Label Uses of Ranitidine Injection
At the forefront of progress, Ranitidine Injection goes beyond its usual applications and ventures into new use areas. This exploration reflects the evolving nature of medical practice, where doctors rely on empirical evidence and clinical expertise to guide their treatment strategies.
- One such unconventional use is in treating hives, where Ranitidine's antihistamine properties are utilized to alleviate symptoms.
- Furthermore, its effectiveness in reducing gastric acid secretion has led to its application in conditions like gastroparesis, characterized by delayed emptying. However, it's important to note that this off-label use remains under clinical scrutiny. A sense of cautious optimism emerges when reviewing the evidence for these nonstandard treatments.
While empirical studies highlight the benefits of using Ranitidine in these unconventional scenarios, the medical community emphasizes the importance of exercising caution and advocates for comprehensive clinical trials to understand its effectiveness and safety in such contexts fully. This careful approach exemplifies the meticulousness with which Ranitidine's therapeutic possibilities are expanded.
How Ranitidine Injection Works
Ranitidine Injection's effectiveness lies in targeting the critical processes involved in stomach acid secretion. This injectable form of Ranitidine showcases innovation as it operates precisely within the complex gastric physiology.
- A vital aspect of its action is inhibiting the histamine H2 receptors found on the parietal cells, which are responsible for acid secretion in the stomach. By blocking these receptors, Ranitidine effectively reduces stomach acid production, relieving symptoms and aiding the healing process of acid-related injuries in the gastrointestinal tract.
- Ranitidine stands out from medications that reduce acidity, especially Proton Pump Inhibitors (PPIs), due to its unique mechanism that targets specific receptors. While PPIs inhibit the step of acid production, Ranitidine's selective blockade of H2 receptors allows for a more controlled decrease in stomach acid levels and potentially results in fewer side effects throughout the body.
This comparison helps us understand where Ranitidine Injection fits into therapy options for managing acid-related disorders. It can be considered an alternative or additional treatment based on patient profiles and clinical goals.
Dosage and Administration Guidelines
The effectiveness of Ranitidine Injection for purposes relies heavily on proper dosage2 and administration. It is crucial to follow established guidelines to achieve the results while minimizing potential risks.
- When treating ulcers and GERD, the recommended dosage is 50 to 150 mg, given through intravenous or intramuscular methods. The actual dosage may vary depending on the severity of the condition. How well the patient responds to treatment.
- In care situations, such as when preventing stress ulcers in critically ill patients, it may be necessary to adjust the dosage and frequency to provide sufficient acid suppression.
- When administering Ranitidine Injection, paying attention to proper techniques is essential. Intravenous administration should be done slowly, either by bolus injection or infusion over time. This is done to prevent fluctuations in drug levels that could affect its effectiveness or cause adverse reactions.
- While joint intramuscular administration can be an alternative route if intravenous access is not feasible or contraindicated.
To summarize, administering Ranitidine Injection requires a customized approach based on the condition being treated, patient characteristics, and a thorough understanding of how the drug works regarding its pharmacodynamics and pharmacokinetics.

Common Side Effects of Ranitidine Injection
Ranitidine Injection, although effective in reducing acid levels, can still cause some reactions. Recognizing and dealing with these side effects is essential for using this medication.
- Common side effects1 of Ranitidine Injection include headaches, dizziness, and gastrointestinal issues like constipation or diarrhea. These symptoms are usually mild and temporary, improving with continued use or slight adjustments in dosage.
- Another set of effects may involve various skin reactions ranging from mild rashes to more noticeable skin problems.
To manage these side effects, healthcare professionals often suggest closely monitoring the dosage and adjusting as needed. They may also recommend treatment to provide relief. Patients should promptly report any persistent or worsening symptoms to their healthcare provider for assistance.

Detailed Analysis of Ranitidine Injection Side Effects
An in-depth examination of the side effects of Ranitidine Injection reveals a range of severe but uncommon reactions that require careful attention and timely intervention.
- These rare and severe side effects include hypersensitivity reactions like anaphylaxis, as well as acute pancreatitis. Immediate medical attention is necessary for these conditions, and in some cases, medication discontinuation may be required.
- There have also been reports of cardiac arrhythmias and changes in blood counts, such as agranulocytosis.
Ongoing clinical research aims to understand the long-term impact of Ranitidine Injection on rare side effects. Risk factors that may make individuals more prone to these reactions include pre-existing medical conditions, concurrent use of other medications, and genetic predispositions. Conducting assessments and closely monitoring patients during their therapy with Ranitidine is crucial. This complex interaction between factors highlights the significance of individualized patient care.
Ultimately, understanding common and rare side effects associated with Ranitidine Injection is essential for optimizing its therapeutic effectiveness while prioritizing patient well-being. Achieving this balance requires clinical oversight, patient education, and a commitment to personalized medicine.
Interactions with Other Medications
Ranitidine Injection, like other medications, doesn't exist in isolation when it comes to clinical use. It interacts with other medicines in a complex therapeutic environment. Understanding and managing its interactions with other drugs is essential to ensure patient safety and treatment effectiveness.
- One key aspect is how Ranitidine can affect the absorption of drugs that rely on stomach acidity levels for optimal results. This means that the impact of Ranitidine on pH can influence the effectiveness of certain medications.
- In addition, significant interactions may occur with medications that are metabolized through the pathways in the liver. This can lead to changes in drug levels, which may cause either toxicity or reduced efficacy.
Given that many patients have health conditions and take multiple medications (polypharmacy), it becomes crucial to manage these interactions effectively. Strategies such as medication reconciliation, dose adjustments, and careful timing of Ranitidine administration relative to other drugs can help minimize risks associated with these interactions.
Warnings and Contraindications
Although it has value, Ranitidine Injection may not be suitable for everyone. It is crucial to identify patients at risk and understanding situations where its use should be avoided in clinical decision-making.
- High-risk patients include those who have had reactions to Ranitidine or similar substances, as well as individuals with specific medical conditions like kidney problems that require dosage adjustments to avoid potentially harmful accumulation.
- It is essential to exercise caution or consider alternatives when using Ranitidine Injection in scenarios involving gastrointestinal conditions. This is because reducing stomach acid levels could mask symptoms and delay diagnosis.
Moreover, it is necessary to assess and monitor patients due to Ranitidine's potential impact on specific lab tests and its long-term implications, such as vitamin B12 deficiency. When contraindications are present, alternative treatments should be considered to ensure effective management of the patient's condition.
Ultimately, the appropriate use of Ranitidine Injection requires an approach that balances its benefits with potential risks while customizing treatment based on individual patient profiles. This approach highlights the importance of patient-centered care in pharmacotherapy.
Careful Administration of Ranitidine Injection
The administration of Ranitidine Injection requires an approach that focuses on the best practices to ensure both effectiveness and safety. This involves a comprehensive strategy that covers various aspects, including determining the appropriate dosage and monitoring the patient's condition.
- One of the best practices is accurately assessing the patient's condition and medical history to determine if Ranitidine is suitable. This includes evaluating risks, benefits, and alternative treatments.
- The method of administering Ranitidine Injection, whether through intramuscular routes, should be chosen based on the patient's specific needs while considering techniques that minimize discomfort and potential complications.
Regular monitoring and treatment adjustment are crucial in managing patients who receive Ranitidine Injection. Assessing symptom improvement, potential side effects, and interactions with other medications is essential. Based on these evaluations, adjustments may be necessary to ensure the therapy remains effective and safe throughout the treatment.
Important Precautions with Ranitidine Injection
Ranitidine Injection is a treatment for various gastric conditions, but it requires following specific safety measures to mitigate risks and improve therapeutic outcomes.
- To ensure safety and personalized care, carefully screen patients for allergies and pre-existing conditions, accurately calculate dosage (especially in individuals with kidney or liver problems) and remain vigilant for adverse reactions. When using Ranitidine Injection in settings, there are additional considerations to remember.
- This includes the potential for drug interactions, how Ranitidine may affect laboratory tests, and evaluating its use in specific patient groups like pregnant or nursing women as well as elderly individuals.
In summary, the responsible administration of Ranitidine Injection and adherence to precautions are crucial in ensuring it serves as a beneficial therapeutic option. These practices demonstrate a commitment to patient safety and individualized care that aligns with clinical standards.
Administration to Specific Populations
The administration of Ranitidine Injection in populations requires a customized approach that considers their unique physiological characteristics and needs.
- When it comes to patients, pregnant women, nursing mothers, and children, specific factors need to be considered when making treatment decisions. For patients, adjustments in dosage and close monitoring are necessary due to physiological changes like decreased renal function. Observing the drug's effectiveness and potential adverse effects is crucial as older adults may have increased sensitivity.
- When it comes to women and nursing mothers, using Ranitidine Injection during pregnancy and lactation requires a careful evaluation of the risks versus benefits. Studies suggest that risk guidelines recommend its use only when necessary while considering the potential impact on the fetus or nursing infant. In the case of use, ensuring safety and efficacy is paramount.
- Dosage must be adjusted based on age and weight, with administration supervised closely by medical professionals. Monitoring response and possible side effects is essential for this vulnerable population.
Handling Overdosage of Ranitidine Injection
Overdosing on Ranitidine Injection is an occurrence, but it can have significant clinical implications that require immediate attention and intervention.
- It's vital to be able to identify the symptoms of an overdose. These symptoms may include a fast heart rate, low blood pressure, and gastrointestinal disturbances. In some cases, you might also experience neurological symptoms like feeling tired all the time, confusion, or even seizures. Recognizing these signs promptly is crucial for management.
- When dealing with an overdose situation, the first step is to stop taking the medication and provide support. Medical interventions may be necessary to prevent absorption of the drug, facilitate its elimination from the body, and provide supportive care for affected organ systems. In cases of overdosage, close monitoring in a medical facility becomes essential to ensure patient safety and promote recovery.
Effectively managing situations involving Ranitidine Injection overdoses highlights the importance of pharmacological care and emphasizes the need for vigilance in both administering and monitoring this medication—especially when dealing with vulnerable populations or potential cases of overdosage.

Storage and Handling Precautions for Ranitidine Injection
It is crucial to properly store and handle Ranitidine Injection to ensure its effectiveness and safety. Following guidelines helps maintain the quality of this medication throughout its shelf life.
- Storing Conditions: Keep Ranitidine Injection at room temperature, away from heat and direct sunlight. If exposed to conditions, the stability of the medication may be compromised, which could affect its therapeutic benefits.
- Protocols for Safe Handling: Preventing contamination when handling the injection is essential. Use techniques during preparation to avoid microbial contamination. Additionally, before administering the solution, inspect it for any particles or changes in color, as these could indicate degradation or contamination.

Conclusion: The Future of Ranitidine Injection in Medical Practice
In summarizing the points of Ranitidine Injection, it is clear that it plays a valuable role as a therapeutic agent in managing conditions related to gastric acid. Its effectiveness and an understood profile of side effects and interactions make it a common choice in gastroenterological treatments.
Looking towards the future,, research and developments surrounding the use of Ranitidine indicate an evolving landscape. Recent investigations into its long-term safety profile and the development of targeted formulations demonstrate a dedication to improving patient care. Additionally, ongoing clinical trials and research are exploring therapeutic uses for this medication, potentially expanding its usefulness in medical practice.
Therefore, the future of Ranitidine Injection lies in refining its usage based on scientific advancements and insights from clinical experience. This path highlights the changing nature of medical science as we strive to provide optimal patient-centered therapies.












