Remicade Infusion
- Introduction to Remicade Infusion
- Comprehensive Overview of Uses
- Exploring Off-Label Uses of Remicade
- Dosage and Administration Guidelines
- Composition and Ingredients of Remicade
- Storage and Handling of Remicade
- Drug Interactions and Contraindications
- Side Effects of Remicade
- Important Safety Information and Warnings
- Special Considerations in Administration
- Managing Overdosage and Emergencies
- Conclusion: The Future of Remicade Therapy
Introduction to Remicade Infusion
Remicade1, also known as Infliximab from a standpoint, represents a remarkable advancement in biological therapy. It is an antibody created to target and counteract tumor necrosis factor-alpha (TNFα), a crucial cytokine involved in the inflammatory process. This therapy has become a cornerstone in treating autoimmune disorders, signaling a new era in personalized medicine.
The journey of Remicade has been characterized by research and extensive clinical trials leading to its approval by the FDA, which stands as a significant milestone in therapeutic innovation. This approval has brought about a shift in how we approach the management of debilitating conditions.

Comprehensive Overview of Uses
The therapeutic range of Remicade1 is wide and varied, mainly used for managing arthritis, an autoimmune disorder that causes chronic inflammation in the joints. Its effectiveness in alleviating symptoms and slowing down the progression of this condition has been well documented. Additionally, Remicade plays a role in treating Crohn's disease and ulcerative colitis, two forms of inflammatory bowel diseases that significantly affect the digestive tract, leading to severe discomfort and systemic complications.
- For arthritis: It helps reduce joint pain and inflammation.
- For Crohn's disease: It aims to decrease inflammation and maintain remission.
- For colitis: It targets healing the lining of the intestines and relieves symptoms.
Apart from these uses, Remicade has also shown effectiveness in treating psoriatic arthritis, ankylosing spondylitis, and plaque psoriasis. Although these conditions have clinical presentations, they share a common underlying factor—chronic inflammation mediated by TNFα. In arthritis, Remicade assists in managing joint pain and skin symptoms. In spondylitis, it helps reduce inflammation in the spine while maintaining mobility. For patients with plaque psoriasis, Remicade offers relief by reducing inflammatory skin lesions.
In care, Remicade has demonstrated promise for children and adolescents when conventional treatments are not effective. Its application in treating rheumatoid arthritis and pediatric Crohn's disease showcases its adaptability and effectiveness among younger individuals, highlighting its potential to shape the course of these conditions during their crucial developmental stages.
Exploring Off-Label Uses of Remicade
The world of using Remicade for purposes not officially approved by the FDA is expanding with possibilities supported by ongoing research and clinical trials. These studies aim to explore the effectiveness of Remicade in treating conditions beyond its approved uses, broadening the range of therapeutic options.
- The basis for these trials lies in understanding how Remicade works at its core, offering the potential for various autoimmune and inflammatory disorders.
- Cutting-edge research is underway to investigate how Remicade could be beneficial in conditions. Rigorous clinical trials are being conducted to ensure that off-label uses of Remicade are safe and effective.
Certain conditions have shown promising results, with Remicade among the possible off-label uses. These include uveitis, Behçets disease, and specific dermatological conditions. While evidence supports its use in these situations, it's essential to approach these off-label applications carefully, weighing benefits against any associated risks.
Understanding How Remicade Works
Remicade's therapeutic effectiveness is rooted in its way of treating autoimmune diseases. By targeting tumor necrosis factor (TNF), a crucial molecule involved in inflammation and immune system imbalance, Remicade effectively mitigates the inflammatory process that plays a significant role in developing different autoimmune disorders.
- Remicade interrupts the inflammatory pathway, relieving symptoms associated with autoimmune diseases.
- TNF inhibitors, like Remicade, play a role in regulating immune responses and reducing inflammation.
Dosage and Administration Guidelines
The way Remicade is prescribed considers each condition's needs, showing a thoughtful approach to treatment. The recommended doses3 vary depending on the disease, the severity of the condition, and how patients respond. This personalized dosing strategy aims to achieve effectiveness while minimizing potential side effects.
- For Rheumatoid Arthritis: The frequency and amount of medication are tailored to meet needs.
- For Crohn's Disease: The dosage is adjusted based on the severity and progression of the disease.
- For Psoriasis: The dosing is adapted according to how the patient responds and tolerates the treatment.
A step-by-step process is followed when administering Remicade through an infusion, usually in a clinical setting. This process begins with preparing the patient and then carefully calculating the dose based on their weight and specific condition. The infusion is given under medical supervision with continuous monitoring for possible adverse reactions. Appropriate post-infusion care is crucial as part of the treatment plan.

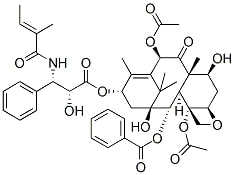
Composition and Ingredients of Remicade
Remicade, an example of biologic medication, comprises active and inactive components carefully designed to regulate the immune system.
- The active ingredient, Infliximab, is a monoclonal antibody created using biotechnology to target and neutralize tumor necrosis factor-alpha (TNFα) specifically. This crucial action disrupts the chain of responses characteristic of autoimmune diseases.
- The inactive ingredients in Remicade, such as sucrose, polysorbate 80, and sodium phosphate, are specifically chosen to stabilize the formulation and improve the medication's solubility and shelf life.
The active ingredient in Remicade is Infliximab, which plays a role in targeting TNFα. The inactive ingredients serve as stabilizers and enhancers for solubility. Understanding the nature of medications like Remicade is essential. Unlike pharmaceuticals that are chemically synthesized, biologics are derived from living organisms. This origin allows them to focus on specific immune system elements, providing a precise therapeutic approach for autoimmune diseases.
Storage and Handling of Remicade
The effectiveness and safety of Remicade greatly depend on how it's stored and handled. It should be refrigerated at a temperature range of 2 8°C (36 46°F) to maintain its stability and strength. It is crucial to protect the medication from light and avoid freezing it, as these factors can cause the active ingredients to degrade. When disposing of Remicade, it is essential to handle it carefully according to the guidelines for disposing of materials. This ensures safety and prevents accidental exposure to this powerful biological agent.
Drug Interactions and Contraindications
It is crucial to have an understanding of the potential drug interactions5 and contraindications associated with Remicade to use it safely and effectively. Remicade has the potential to interact with medications, which may affect its effectiveness or increase the risk of adverse effects. In particular, using Remicade with other immunosuppressants like methotrexate can increase the chances of immunosuppression. It is also essential to avoid administering vaccines while undergoing treatment with Remicade because the weakened immune response could lead to inadequate vaccine efficacy and potential complications.
- There are everyday drug interactions, including those with immunosuppressants, live vaccines, and certain antibiotics.
- On the other hand, there are specific contraindications that should be considered as well. These include allergies to Infliximab or any other components of Remicade, certain infections, and specific medical conditions.
Certain conditions contraindicate the use of Remicade. These include hypersensitivity reactions to Infliximab or any other component of the medication. Additionally, patients with tuberculosis, certain fungal infections, or other severe infections should not receive treatment with Remicade. These contraindications highlight the importance of evaluating each patient's medical history before starting therapy.

Side Effects of Remicade
The administration of Remicade, like any treatment, can have a range of possible side effects, varying in severity. Common side effects2 often include symptoms such as headaches, nausea, and reactions related to the infusion process, like fever and chills. These symptoms are usually mild to moderate. It can be managed without the need for additional intervention.
- Some examples of milder effects are headaches, nausea, and infusion reactions.
- However, there is a possibility of experiencing side effects for patients, including severe infections due to a suppressed immune system, hypersensitivity reactions, or potential liver damage.
It is crucial for healthcare providers to closely monitor patients for these reactions and take immediate action if they occur. Managing side effects requires collaboration between patients, caregivers, and healthcare professionals. Effective management can involve staying hydrated and promptly reporting any symptoms experienced by the patient while strictly adhering to pre-medication protocols to mitigate infusion-related reactions.

Important Safety Information and Warnings
Remicade comes with safety warnings, particularly highlighted in the black box warnings. These warnings emphasize the increased risk of infections like tuberculosis and sepsis as well as the possibility of developing malignancies such as lymphoma. It is crucial for patients who receive Remicade to undergo screening for diseases and to be consistently monitored for signs of malignancy. The monitoring process during Remicade treatment is thorough. Regular health assessments, blood tests, and imaging studies are involved in proactively detecting potential complications.

Special Considerations in Administration
When administering Remicade, it is essential to consider factors such as the patient's age, pregnancy status, and pediatric requirements.
- Elderly individuals may have a vulnerability to infections and a slower response to treatment, so close monitoring and potential dosage adjustments are necessary.
- For women and nursing mothers, the decision to use Remicade should be carefully evaluated in terms of potential risks to the fetus or infant.
- It is still essential to customize the treatment according to each child's needs by monitoring their growth and development and making dosage adjustments when needed.
Although studies are limited, it is crucial to consider the effects on the immune system and consult closely with healthcare professionals. Remicade has been proven safe and effective for certain conditions in patients.
Managing Overdosage and Emergencies
When someone takes too much Remicade, it's crucial to recognize and manage the situation quickly. One may experience worsened side effects like allergic reactions or increased infection vulnerability. It is essential to identify these signs to prevent any severe complications.
- Symptoms of overdosage include intensified side effects such as hypersensitivity and a higher risk of infection.
If an emergency arises, immediate medical attention is necessary. There are no remedies for Remicade overdosage, so the treatment primarily focuses on providing support and managing symptoms. Healthcare professionals should prioritize stabilizing the patient, monitoring their signs, and addressing specific symptoms through appropriate interventions.
Precautions in Handling and Administration
It is crucial to prioritize Remicade's handling and administration, especially considering the risk of infections associated with immunosuppressive agents. When preparing and administering infusions, healthcare providers must follow infection control practices, including aseptic techniques. To minimize the risk of infection, adhering to protocols for handling infusions and carefully monitoring patients during the administration process is essential.
In settings where Remicade infusions are handled, great attention to detail is required to ensure that patients are safe and treatment is effective. This involves storing, preparing, and disposing of the medication and closely monitoring patients both during and after the infusion.
Conclusion: The Future of Remicade Therapy
Looking ahead, there is dynamic research and potential advancements in Remicade therapy. Studies are currently being conducted to explore and refine dosing strategies and investigate long-term outcomes to improve its therapeutic impact. Exciting developments include the possibility of combining therapies, personalized medicine approaches and improvements in how it's administered.
Continued research aims to expand the range of conditions Remicade can effectively treat while optimizing its effectiveness. There are promising advancements in medicine and the potential for combining different treatments. To sum up, Remicade remains an aspect of modern medicine, especially in managing autoimmune disorders. Its significance will likely grow as further research offers treatment options and hope for patients worldwide. The journey of Remicade from its inception until now reflects the evolution of medical science and our unwavering commitment to improving patient care.










