Tirofiban
- I. Introduction
- II. Composition of Tirofiban
- III. How Tirofiban Works
- IV. Uses of Tirofiban
- V. Dosage and Administration
- VI. Side Effects of Tirofiban
- VII. Interaction with Other Drugs and Substances
- VIII. Warnings and Contraindications
- IX. Important Precautions and Careful Administration
- X. Special Administration Guidelines
- XI. Overdose and Management
- XII. Storage and Handling Precautions
I. Introduction
Brief Overview of Tirofiban
Tirofiban is a medication commonly used to prevent blood clot formation during procedures. It works by stopping platelets from sticking, which helps reduce the risk of thrombus formation.
Importance in the Medical Field
Tirofiban plays a role in the healthcare industry by helping to reduce cardiovascular risks, especially when it comes to the formation of blood clots in the coronary arteries. It is a tool for healthcare professionals in their fight against cardiovascular diseases, a significant cause of death worldwide.
Objective of the Article
The main focus of this article is to provide a detailed explanation of different facets related to Tirofiban. It covers topics such as the makeup and how it works, approved uses by the FDA, off-label applications, potential side effects, and recommendations for safe usage.
II. Composition of Tirofiban
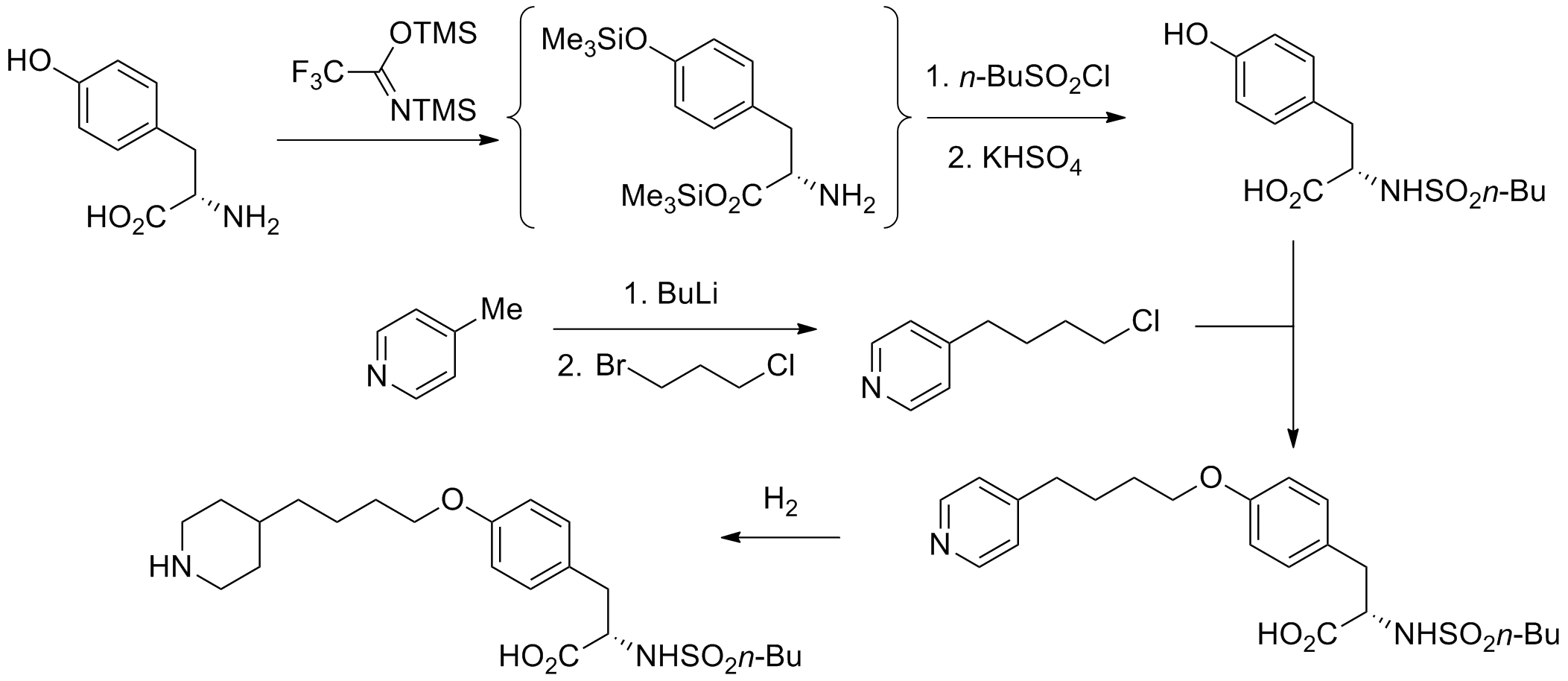
Chemical Structure
Tirofiban possesses a chemical arrangement predominantly consisting of nonpeptide compounds. This particular molecular structure contributes to its specificity and effectiveness.
Active and Inactive Ingredients
Active Ingredient: Hydrochloride Other ingredients commonly found in the formulation include Sodium citrate, citric acid, and polysorbate, often added as excipients.
Pharmaceutical Formulations
Tirofiban is usually found in forms allowing for a quick response in urgent medical situations.
III. How Tirofiban Works
Mechanism of Action
Tirofiban works by blocking the glycoprotein IIb/IIIa receptor, which plays a role in platelet aggregation.
Target Receptors and Pathways
It specifically focuses on the areas where fibrinogen binds to the receptors known as glycoprotein IIb/IIIa on the membrane of platelets.
Pharmacokinetics and Pharmacodynamics
The medication is quick. It is distributed throughout the body. Its life requires it to be continuously infused to ensure the correct levels for effective treatment.
IV. Uses of Tirofiban
FDA-Approved Indications
Acute Coronary Syndrome
Tirofiban is a glycoprotein IIb/IIIa inhibitor used in treating acute coronary syndrome (ACS) and as an adjunct to percutaneous coronary intervention (PCI) 1. It is indicated to reduce the rate of thrombotic cardiovascular events (combined endpoint of death, myocardial infarction, or refractory ischemia/repeat cardiac procedure) in non-ST elevation ACS 1. Tirofiban is inferior to abciximab in treating patients with ACS undergoing PCI 2.
1: Aggrastat (tirofiban) dosing, indications, interactions, adverse effects, and more Drugs & Diseases 2: Antiplatelet therapy in percutaneous coronary intervention
Percutaneous Coronary Intervention
Tirofiban is a medication used to prevent complications caused by reduced blood flow during percutaneous coronary intervention (PCI) 1. It is indicated for the prevention of major cardiovascular events in adult patients presenting with acute coronary syndromes without ST elevation (NSTE-ACS) with the last episode of chest pain occurring within 12 hours and with ECG changes and/or elevated cardiac enzymes 1. Tirofiban is also indicated for the reduction of major cardiovascular events in NSTE-ACS patients planned to undergo PCI within the first 4 hours of diagnosis or STEMI patients undergoing primary PCI 1. Tirofiban should be given in combination with fondaparinux (or enoxaparin), aspirin, and clopidogrel (or ticagrelor). Patients undergoing PCI should receive unfractionated heparin 1.
Here are some references that provide more information about Tirofiban treatment during PCI:
- Tirofiban in Acute Coronary Syndrome - Gloucestershire Hospitals NHS Trust
- Antithrombotic therapy for elective percutaneous coronary intervention - UpToDate
- Tirofiban Monograph for Professionals - Drugs.com
Off-Label Uses
Stroke Management
Tirofiban is a medication used to prevent complications caused by reduced blood flow during percutaneous coronary intervention (PCI) 1. It is indicated for the prevention of major cardiovascular events in adult patients presenting with acute coronary syndromes without ST elevation (NSTE-ACS) with the last episode of chest pain occurring within 12 hours and with ECG changes and/or elevated cardiac enzymes 1. Tirofiban is also indicated for the reduction of major cardiovascular events in NSTE-ACS patients planned to undergo PCI within the first 4 hours of diagnosis or STEMI patients undergoing primary PCI 1. Tirofiban should be given in combination with fondaparinux (or enoxaparin), aspirin, and clopidogrel (or ticagrelor). Patients undergoing PCI should receive unfractionated heparin 1.
There are some studies that suggest tirofiban may be effective in treating acute ischemic stroke patients with large artery atherosclerosis stroke etiology undergoing endovascular therapy 21. However, the safety and efficacy of tirofiban for patients with acute ischemic stroke (AIS) remains controversial 2. Further studies are needed to determine its efficacy post-endovascular therapy 2.
Here are some references that provide more information about Tirofiban treatment during PCI and its use in AIS:
- Tirofiban Monograph for Professionals - Drugs.com
- Antithrombotic therapy for elective percutaneous coronary intervention - UpToDate
- Safety and Efficacy of Tirofiban for Acute Ischemic Stroke Patients With Large Artery Atherosclerosis Stroke Etiology Undergoing Endovascular Therapy - Frontiers in Neurology
- Tirofiban for Stroke Without Large or Medium Vessel Occlusion - American College of Cardiology
- Efficacy outcomes and safety measures of intravenous tirofiban or oral clopidogrel as adjunctive therapy after endovascular thrombectomy for acute ischemic stroke - Journal of Thrombosis and Thrombolysis
- Safety and Efficacy of Tirofiban During Intravenous Thrombolysis or Endovascular Treatment for Acute Ischemic Stroke: A Systematic Review and Meta-Analysis - Frontiers in Neurology
Peripheral Arterial Disease and Deep Vein Thrombosis
Tirofiban is a medication used to prevent complications caused by reduced blood flow during percutaneous coronary intervention (PCI) 1. It is indicated for the prevention of major cardiovascular events in adult patients presenting with acute coronary syndromes without ST elevation (NSTE-ACS) with the last episode of chest pain occurring within 12 hours and with ECG changes and/or elevated cardiac enzymes 1. Tirofiban is also indicated for the reduction of major cardiovascular events in NSTE-ACS patients planned to undergo PCI within the first 4 hours of diagnosis or STEMI patients undergoing primary PCI 1. Tirofiban should be given in combination with fondaparinux (or enoxaparin), aspirin, and clopidogrel (or ticagrelor). Patients undergoing PCI should receive unfractionated heparin 1.
There are some studies that suggest tirofiban may be effective in treating acute ischemic stroke patients with large artery atherosclerosis stroke etiology undergoing endovascular therapy 1. However, the safety and efficacy of tirofiban for patients with acute ischemic stroke (AIS) remains controversial . Further studies are needed to determine its efficacy post-endovascular therapy .
- Tirofiban Monograph for Professionals - Drugs.com
- Evolving Treatments for Arterial and Venous Thrombosis - AHA/ASA Journals
- Unexplained arterial thrombosis: approach to diagnosis and treatment - Hematology
V. Dosage and Administration
Standard Dosage Recommendations
The usual recommended dosage involves administering an injection through a vein followed by a continuous infusion.
Adjustments for Specific Populations
Certain groups of individuals, like the elderly or those with kidney problems, might need to adjust their dosages.
Route of Administration
The effective way to achieve rapid results is through intravenous administration.
Importance of Medical Supervision
It is crucial to have medical supervision to observe for any possible adverse reactions and make necessary adjustments to the dosage.
VI. Side Effects of Tirofiban
Common Side Effects
- Bleeding
- Bruising
- Nausea
Serious Side Effects
- Thrombocytopenia
- Hypotension
- Allergic Reactions
VII. Interaction with Other Drugs and Substances
Potential Drug-Drug Interactions
Anticoagulants: There is a chance of bleeding when taking them. Antiplatelet Agents: They can enhance the effect of preventing platelet aggregation. Beta Blockers; They may potentially have a lowering impact on blood pressure.
Substance Interactions
Alcohol consumption can potentially worsen the risks of bleeding. It is important to note that certain herbal supplements, such as Ginkgo Biloba, might also elevate the chances of bleeding.
VIII. Warnings and Contraindications
Absolute Contraindications
- Bleeding Disorders
- Recent Surgery
- Liver Disease
Relative Contraindications
- Kidney Dysfunction
- Age-Related Factors
IX. Important Precautions and Careful Administration
Monitoring During Treatment
It is crucial to monitor the patient's physiological parameters while administering Tirofiban. This includes keeping track of their status, coagulation profile, and renal and hepatic functions.
Laboratory Tests to Consider
In addition to being vigilant in settings, doctors often need to perform specific laboratory tests, such as Complete Blood Count (CBC), Liver Function Tests (LFTs), and Kidney Function Tests (KFTs).
Signs of Adverse Reactions
Immediate medical attention is necessary if there are indications of adverse reactions, such as uncontrollable bleeding, a decrease in platelet count, or allergic responses.
X. Special Administration Guidelines
Administration to the Elderly
Dose Adjustments
As we age, our bodies undergo changes that require us to adjust medication dosages accordingly. This often means starting with initial doses and gradually increasing them as needed.
Risks and Precautions
Older people are often sensitive to blood-thinning medications, which increases their chances of experiencing adverse effects such as bleeding or a decrease, in platelet count.
Administration to Pregnant Women and Nursing Mothers
Potential Risks to Fetus or Infant
Tirofiban administration is classified as a category C pregnancy risk. Essentially research conducted on animals has indicated adverse effects, but there is a lack of human studies to confirm this.
Alternative Treatment Options
Pediatric Dosage
When it is necessary to administer Tirofiban to pediatric patients, the dosage should be tailored specifically for each child. This involves considering the child's weight, age, and medical condition. If possible, it is essential to rely on pharmacokinetic studies to inform this decision-making process.
XI. Overdose and Management
Symptoms of Overdose
Excessive use of Tirofiban can lead to various harmful symptoms, with the most severe being uncontrollable bleeding.

Immediate Steps for Management
It is crucial to stop the drug infusion. At the time, taking hemostatic measures, such as initiating platelet transfusions may be necessary.
Antidotes and Reversal Agents
Although there is no antidote for an overdose of Tirofiban, the primary focus in managing such cases is to provide supportive measures. These measures may involve administering procoagulants, stabilizing the patient's hemodynamics, and closely monitoring them in a care setting.
XII. Storage and Handling Precautions
Optimal Storage Conditions
Storing Tirofiban at room temperature is vital, avoiding any drastic changes in heat or humidity.
Shelf Life
The usual practice is to indicate the expiration date on the packaging of pharmaceuticals. Exceeding this date can jeopardize the effectiveness and safety of the medication.
Disposal Guidelines
Improper disposal of Tirofiban can have impacts on the environment. It is important to follow regulations for disposing of pharmaceuticals properly. This typically involves options like participating in drug take-back programs or incinerating the medication under controlled conditions. The use of Tirofiban in the field of medicine is complex. It requires careful attention to ensure it is administered safely. Healthcare professionals must understand potential interactions, contraindications, and specific considerations for certain patient populations. By following the guidelines outlined here, doctors can maximize the benefits of Tirofiban while minimizing any associated risks.