Cilodoc, Cilostazol
- Introduction
- Composition and Formulation
- How Cilodoc (Cilostazol) Works
- Cilostazol Uses
- Off-Label Uses
- Cilostazol Dosage and Administration
- Cilostazol Side Effects
- Cilostazol Interactions
- Contraindications for Cilodoc (Cilostazol)
- Cilostazol Warnings and Precautions Before Using Cilodoc (Cilostazol)
- Special Populations and Cilostazol Contraindications
- Overdosage and Emergency Management
- Storage and Handling Precautions
Introduction
The drug Cilodoc contains cilostazol and is widely used to treat peripheral arterial disease (PAD) and intermittent claudication, by improving blood flow and reducing platelet aggregation, in the body's cardiovascular system. The medication is categorized as an antiplatelet agent. Also has effects that give it a dual therapeutic purpose. Cilostazol was first created in Japan and has now been approved for use, in various regions worldwide such as the United States and Europe. Its distinct way of working has established it as a substitute to antiplatelet drugs specifically for individuals, with impaired peripheral circulation.
Composition and Formulation
Active Ingredients and Their Functions
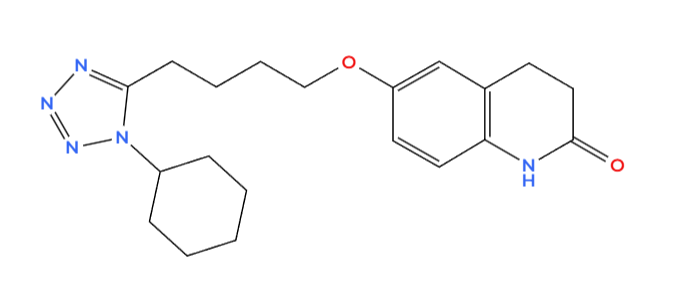
The main component is cilostazol itself, which acts as a PDE-3 inhibitor to widen blood vessels and decrease the clumping of platelets.
Available Strengths and Dosage Forms
Tablets are usually found in 50 mg and 100 mg doses, and they are available for consumption. Extended release versions of formulations provide adjusted release characteristics to enhance the profiles.
Excipients and Inactive Ingredients
Each form of medication contains ingredients that help maintain the drugs effectiveness and availability, in the body while ensuring that patients can easily follow their regimen.
- Microcrystalline Cellulose improves the form and durability of tablets.
- Lactose monohydrate is used as a filler to ensure the tablets are properly composed.
- Hypromellose helps regulate the release of medicine, in formulations.
- Magnesium Stearate functions, as a lubricant to facilitate manufacturing procedures.
How Cilodoc (Cilostazol) Works
Cilostazol Mechanism of Action as a Phosphodiesterase-3 (PDE3) Inhibitor
In a manner Cilostazol hinders phosphodiesterase-3 (PDE3) an enzyme that breaks down cyclic adenosine monophosphate (cAMP). By impeding the degradation of cAMP the medication boosts the levels of cAMP resulting in a series of reactions that improve vascular performance and blood clotting abilities.
..png)
Effects on Blood Vessels and Circulation
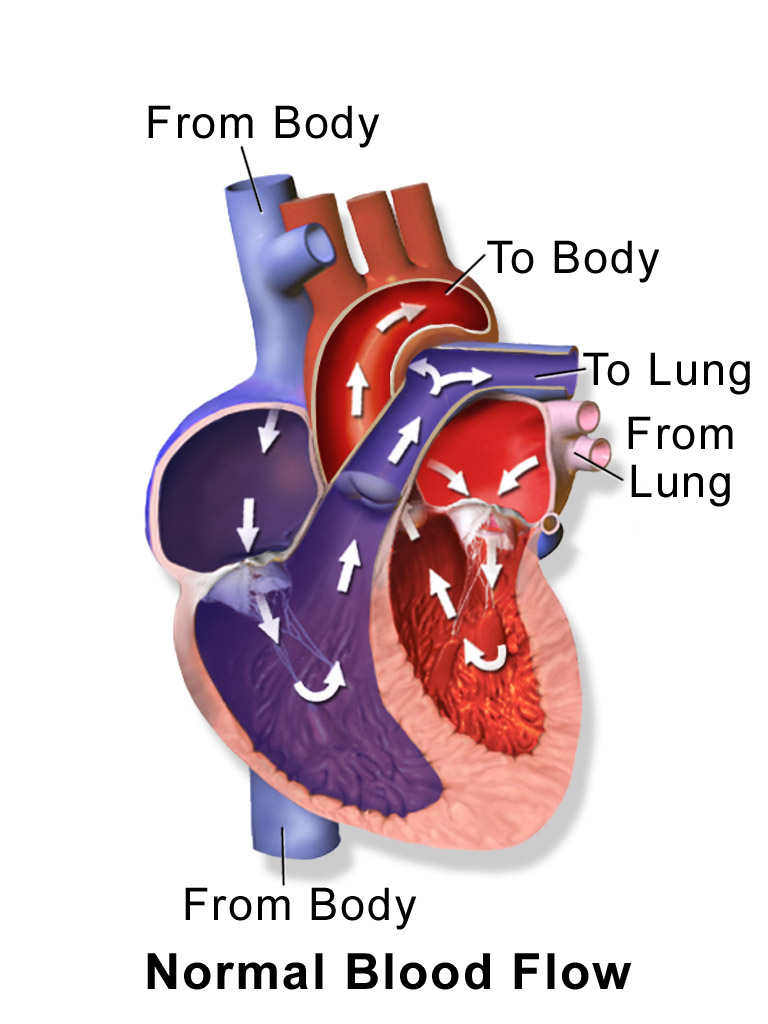
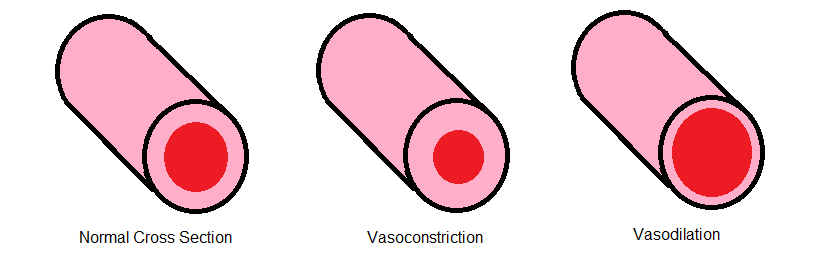
The increased levels of cAMP encourage the relaxation of muscle cells and result in the dilation of arteries—a process that supports a more expansive blood flow, within the body. Enhances the flow of oxygen blood to tissues deprived of oxygen supply. It helps to lower resistance and alleviate symptoms of claudication. Improves the function of blood vessel linings to support heart health.
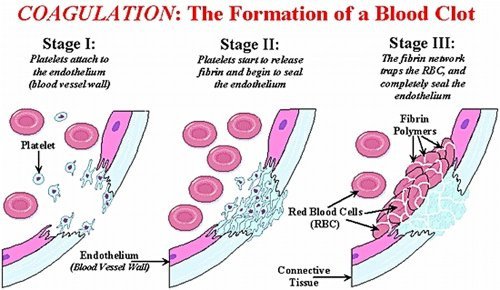
Role in Platelet Aggregation Inhibition
Cilostazol works differently from blood thinners as it can reduce activity without impacting clotting factors significantly through increasing cAMP levels, in platelets. It stops platelets from getting active. Lowers the chances of blood clot formation. Limits the binding of fibrinogen, to receptors, on platelets which reduces their aggregation. When used together with medications that prevent platelet aggregation it enhances their effectiveness through a combined action.
Differences from Other Antiplatelet and Vasodilator Medications
Compared to medications used for issues, cilostazol has a distinct pharmacodynamic profile.
- Aspirin and Clopidogrel work by preventing blood clotting through mechanisms without causing a notable widening of blood vessels.
- Although dipyridamole is a PDE inhibitor, like cilostazol, with a range of effects; it does not cause vasodilation to the same extent as cilostazol does.
- Nitroglycerin and other vasodilators work differently from cilostazol as they do not directly release nitric oxide but instead induce vasodilation through cAMP mediated pathways.
- Cilostazol plays a role, in treating artery disease (PAD) and associated circulatory conditions by blending anti-clotting and blood vessel dilation effects into one compound.
Cilostazol Uses
Primary Indications
Cilostazol is a kind of medicine that falls under the category of phosphodiesterase (PDE inhibitor), commonly used in the field of medicine for its ability to work in two ways at once. It helps by preventing blood clotting and widening blood vessels which is important, for blood flow and lowering the risk of blood clots forming. This medicine is most helpful for people with issues related to circulation in their arms or legs well, as those who are more likely to have strokes.

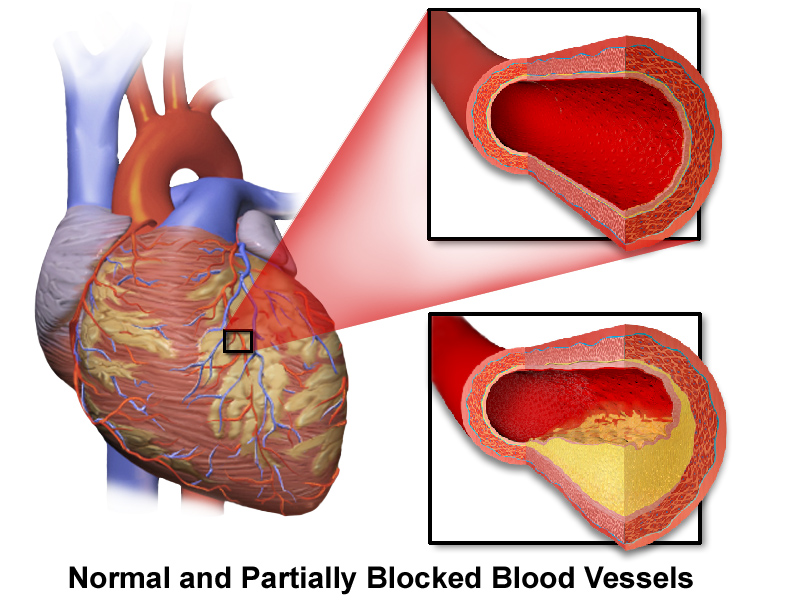
Treatment of Intermittent Claudication in Peripheral Arterial Disease
Cilostazol is widely recognized for its effectiveness in treating claudication associated with peripheral arterial disease (PAD). This condition causes cramping in the legs due to reduced blood flow, from narrowed arteries—an issue seen in PAD patients.
Cilostazols distinct pharmacological characteristics provide advantages in managing PAD symptoms;
- Improving Walking Distance Benefits Seen in Studies show enhancements, in pain maximum walking distances for individuals, with intermittent claudication.
- Peripheral Artery Vasodilation: Blocking PDE3 boosts the levels of cAMP inside cells, causing the muscles, in blood vessels to relax and allowing the arteries to widen.
- Improvement, in ischemic symptoms is achieved through enhanced blood flow, to the extremities by cilostazol, which helps reduce pain and boosts patient mobility and overall quality of life.
- Cilostazol dilates blood vessels. Also protects endothelial cells by reducing oxidative stress and enhancing the availability of nitric oxide.
Given these impacts cilostazol is commonly recommended as a component of a plan, for managing PAD along with changes, in lifestyle and antithrombotic treatment.
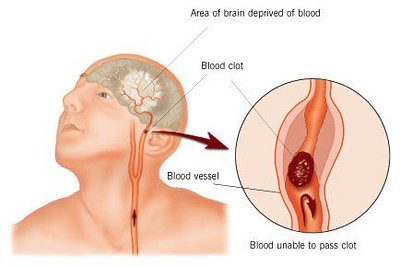
Prevention of Stroke and Cardiovascular Events in Specific Populations
Cilostazol has been gaining recognition not only for its effectiveness in PAD but also for its potential in preventing strokes in individuals who have experienced non-cardioembolic ischemic strokes before.
This medications ability to prevent platelet aggregation plays a role in lowering the risk of recurring events when compared to conventional antiplatelet medications, like aspirin and clopidogrel. Some important points to note about cilostazol regarding stroke prevention and reducing events are as follows;
- Platelet Aggregation Inhibition Clarification; Cilostazol differs from cyclooxygenase inhibitors by blocking PDE3 selectively.
- Chosen reactions, in platelets and causing a temporary decrease, in platelet activation.
- Cilostazol offers an impact on blood circulation without the added risk of bleeding often associated with antiplatelet medications.
- The research indicates that cilostazol could be advantageous, for individuals with narrowing of the arteries, inside the brain when conventional antiplatelet treatments may not be as effective.
In groups of people, at risk of recurring blockages in the blood vessels but also needing to reduce the chance of bleeding complications after a stroke to prevent future incidents. Cilostazol plays a crucial role in preventing secondary strokes effectively and safely. By managing both issues related to blood circulation in the limbs and the risk of strokes in the brain, cilostazol remains a treatment option in today's advanced cardiovascular healthcare system.
Off-Label Uses
Secondary Stroke Prevention
Cilostazol is typically used for treating intermittent claudication. It has shown potential, in preventing secondary strokes due to its unique phosphodiesterase three (PD-3) inhibition properties that reduce platelet aggregation and promote vasodilation to lower the risk of recurrent ischemic events in patients, with noncardioembolic stroke history. Potential advantages of using cilostazol in stroke care may include;
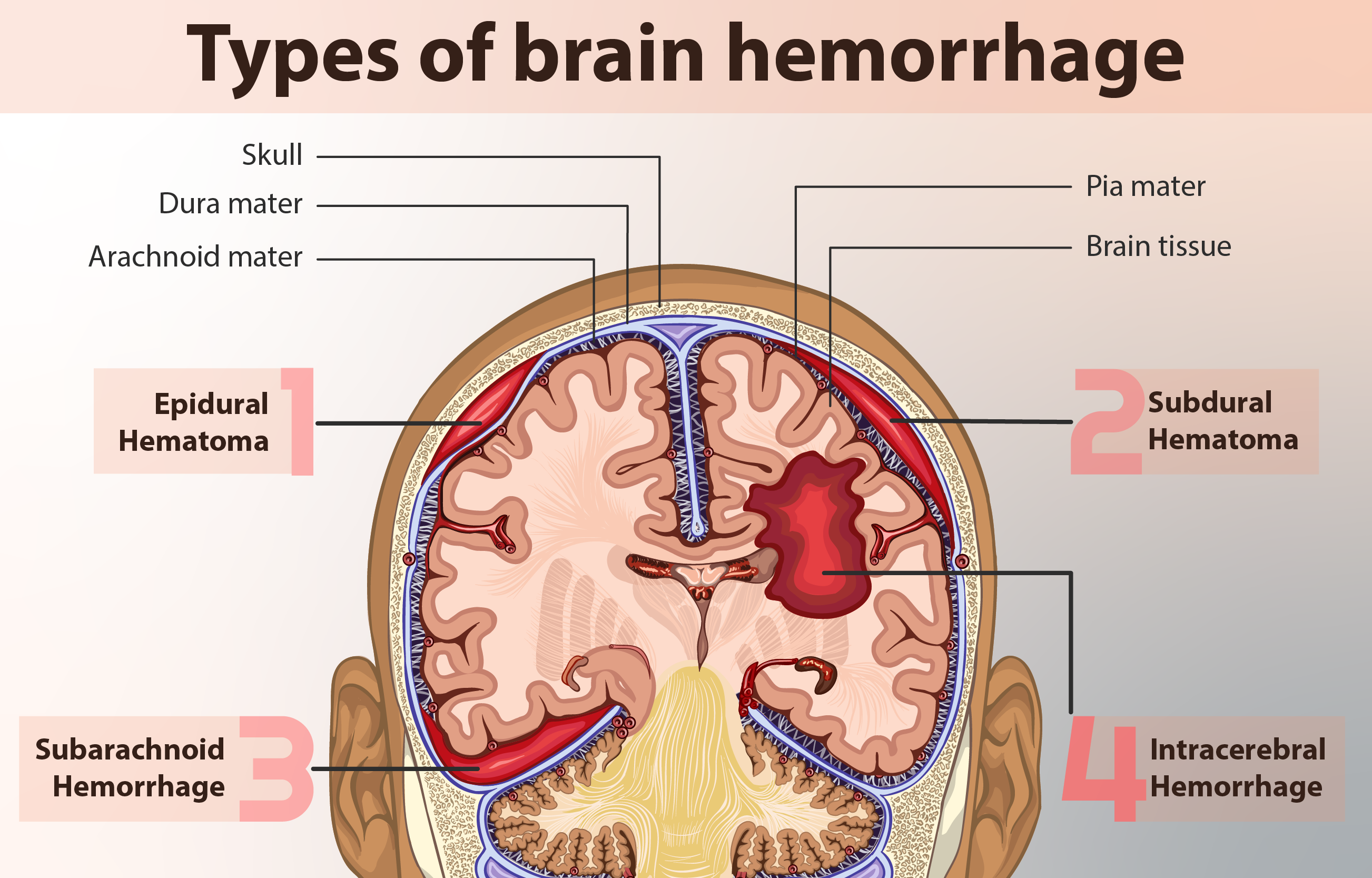
- Cilostazol may present a risk of hemorrhage when compared to traditional antiplatelet medications, like aspirin.
- Improved Blood Circulation, in the Brain; The ability of cilostazol to widen blood vessels helps enhance blood flow to areas of the brain affected by reduced blood supply due, to ischemia may assist in the recovery of functions.
- Cilostazols capability to regulate function could potentially help mitigate inflammation and the advancement of atherosclerosis, in blood vessels.
Cilostazol is being commonly used as a complementary treatment for certain individuals who need ongoing stroke prevention with a careful evaluation of the risks and benefits involved.
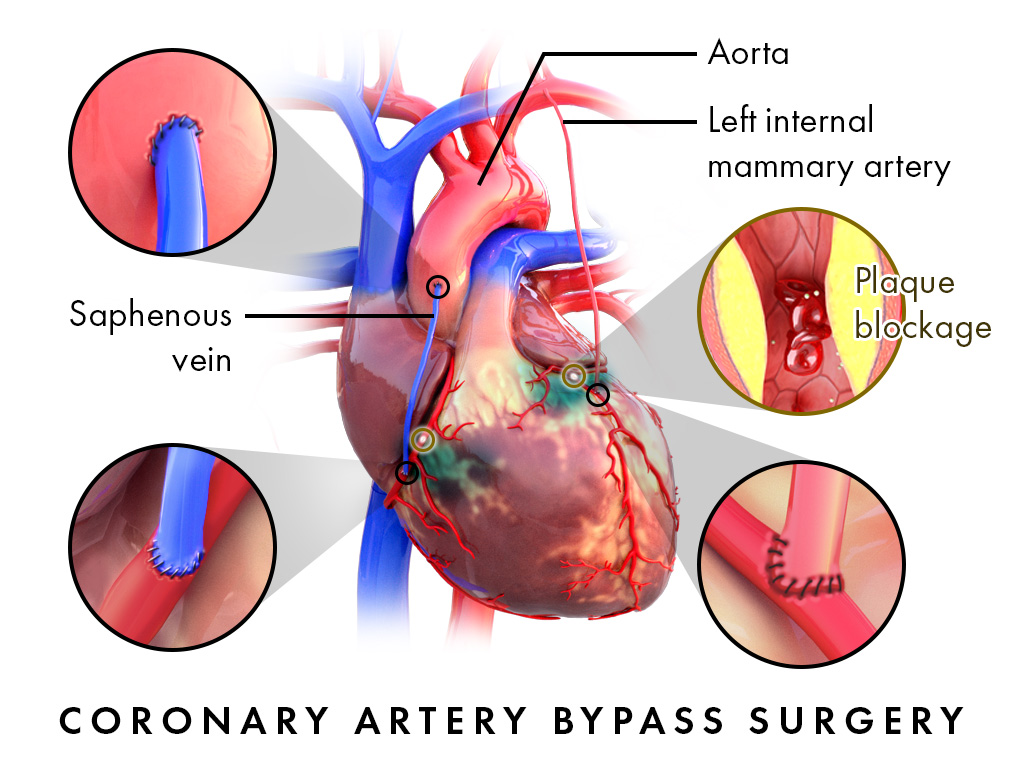
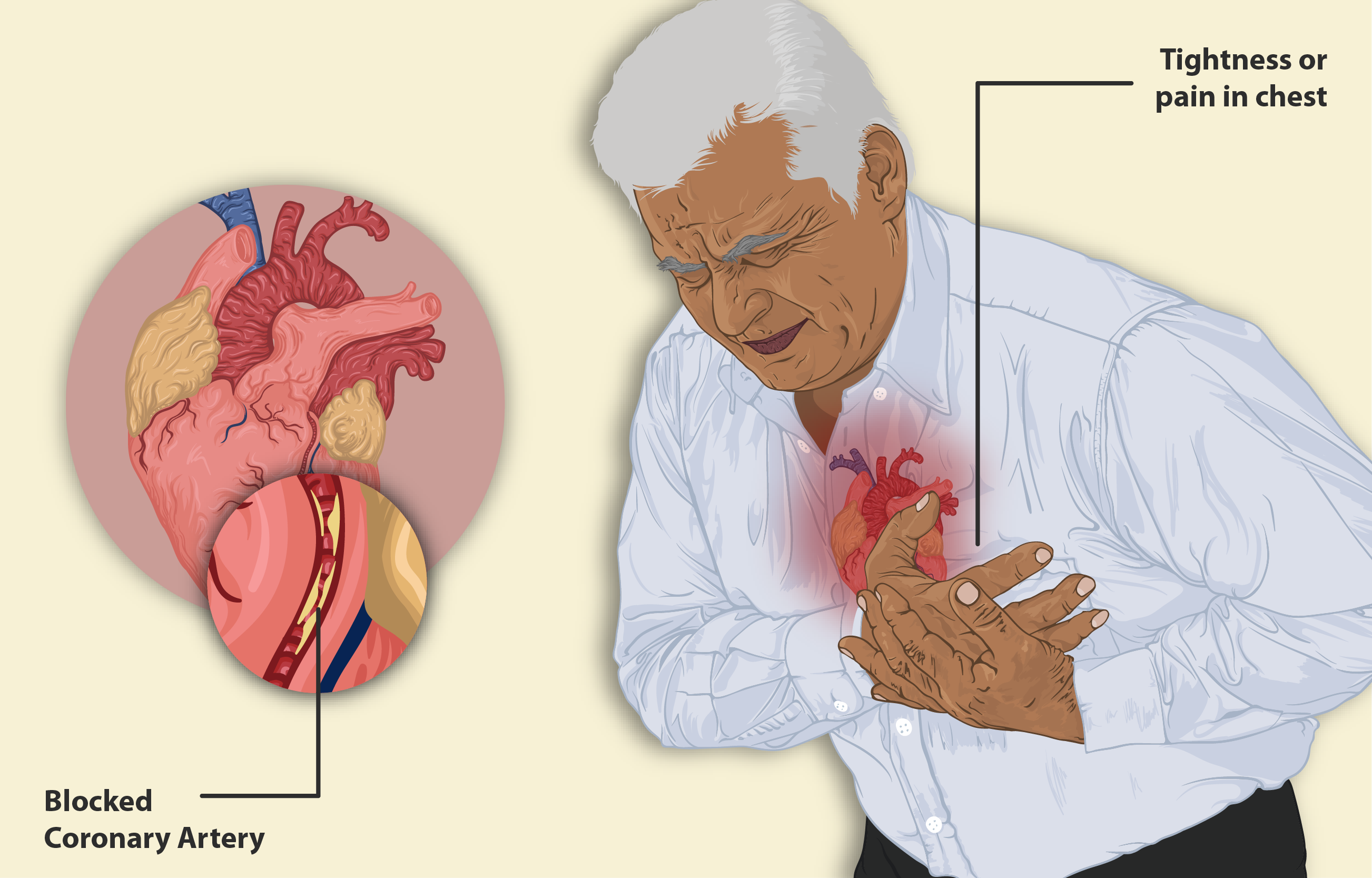
Treatment of Ischemic Heart Disease
While cilostazol is not typically the treatment, for ischemic heart disease (IHD), studies have shown its promising potential in enhancing the function of coronary microvasculature by promoting vasodilation and preventing platelet aggregation thereby offering theoretical advantages for managing chronic stable angina and microvascular angina. Cilostazols off label use in IHD is supported by mechanisms such, as these;
- Enhancing the relaxation of arteries through an increase in intracellular cAMP levels allows cilostazol to improve the oxygen supply to the myocardium by inducing coronary vasodilation.
- Emerging studies indicate that cilostazol could be beneficial, for individuals, with flow or endothelial dysfunction, potentially reducing microvascular dysfunction.
- Exploring Additional Treatment in the Revascularization Process; Certain research has looked into how it can improve the function of blood vessel walls after a procedure, like angioplasty.
Additional research is necessary to confirm its effectiveness and explore its benefits further in treating ischemic heart disease.
.webp)
Management of Chronic Limb Ischemia
The importance of Cilostazol, in treating peripheral arterial disease (PAD) is widely acknowledged; however, it may also be beneficial in addressing serious cases like chronic limb-threatening ischemia (CLTI). This condition is characterized by rest pain due to blood flow and slow-healing ulcers that require immediate and proactive treatment. Possible benefits, in managing CLTI;
- Enhanced Blood Flow, in Blood Vessels: The widening of blood vessels improves the flow in circulation and could possibly postpone the requirement for surgery.
- Enhanced blood circulation might help reduce ischemic pain in individuals, with peripheral artery disease (PAD).
- Supplement to Revascularization Procedure Benefits; Cilostazol could improve results, for individuals receiving bypass surgery.
In treating chronic limb-threatening ischemia (CLTI) traditional treatments are important; however the pharmacological effects of cilostazol provide a reason to include it in holistic vascular care.
Use in Cerebrovascular Disorders
Research is currently exploring cilostazols effects on conditions, like vascular dementia and cerebral small vessel disease (CSVD) in addition to its known benefits in preventing strokes. Several possible mechanisms suggest its benefits, for health.
- Enhanced Blood Circulation, in the Brain; The widening of blood vessels could help increase the supply of oxygen to areas of the brain, with reduced blood flow.
- Cilostazol has the potential to protect the brain by having anti-inflammatory and antioxidant properties, which could help prevent cognitive decline.
- Some research indicates that cilostazol might help lower the chances of having another lacunar stroke by protecting the health of blood vessels.
Ongoing studies suggest that cilostazol could potentially play a role in treating cerebrovascular insufficiency and associated neurological disorders.
Potential Role in Diabetic Neuropathy
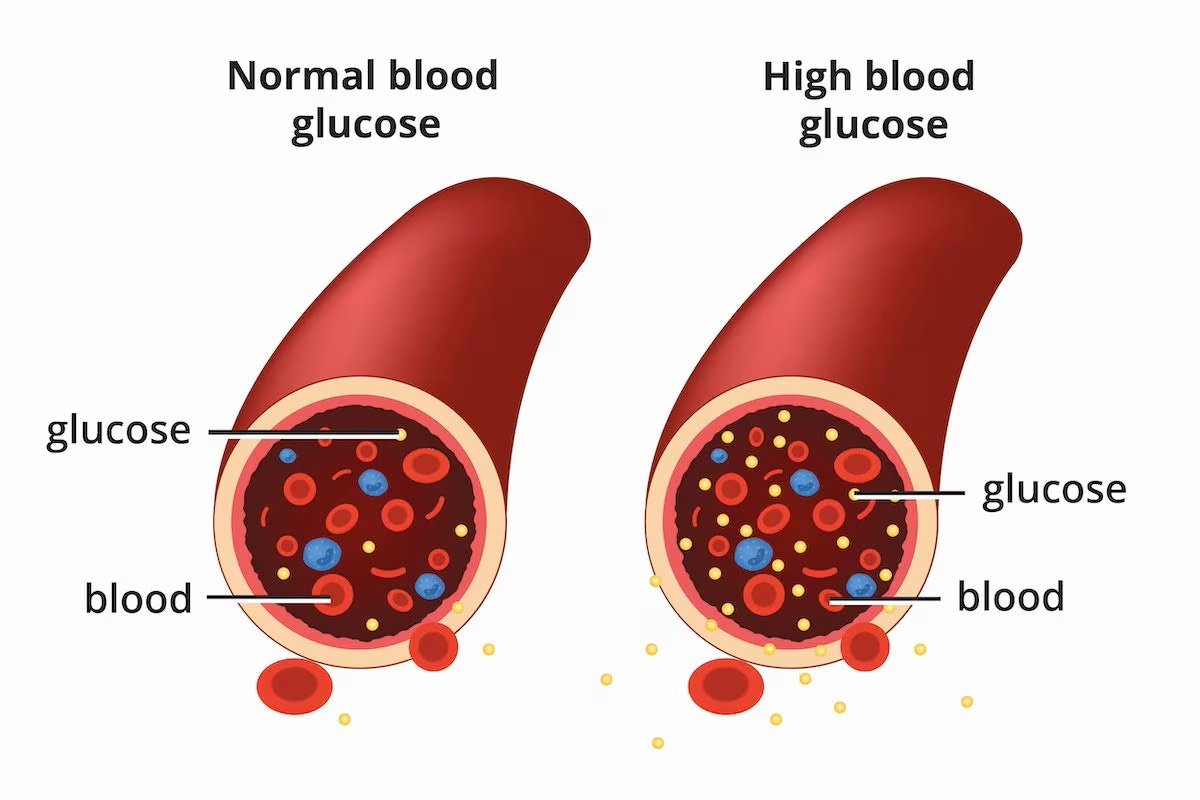
Diabetic neuropathy is an issue that arises from high blood sugar levels and involves problems, with tiny blood vessels and nerve damage. Cilostazol seems to have advantages than its impact on blood vessels, in addressing this condition by enhancing how the cells lining the blood vessels work and boosting nerve blood supply. Potential ways cilostazol could help with neuropathy;
- Reviving Microcirculation; The dilation of blood vessels could potentially offset the harm caused by blood flow, in the nerves on the parts of the body.
- Reduction of Oxidative Stress: Cilostazols antioxidant properties may help reduce inflammation in the nerves.
- Enhancement of Sensory Function; Initial research suggests an involvement, in easing discomfort and reestablishing sensory awareness.
While not widely used as a therapy for neuropathy at present, cilostazol offers a fresh direction, for exploring neurovascular defense in research.

Cilostazol Dosage and Administration
Cilostazol Dosing
The prescribed amount of cilostazol is precisely adjusted to maximize its ability to widen blood vessels and prevent blood clotting while reducing the risk of side effects. Standardized dosages are, in place to guarantee effectiveness in treating conditions like peripheral arterial disease (PAD), ensuring optimal results for patients, with vascular issues.
Recommended Dosage for Intermittent Claudication
For treating claudication linked to artery disease (PAD) the typical recommended dose of cilosazol is;
- Take 100 milligrams two times a day by mouth.
- Consider using doses, such, as 50 mg taken twice a day for patients who may be more prone, to experiencing side effects.
Scheduled administration helps increase blood circulation to areas, with reduced blood flow due to restricted blood vessels in limbs affected by oxygen supply during physical activity or rest periods and reduces discomfort while walking and enhances the ability to engage in physical activities for longer durations without discomfort gradually becoming noticeable within 2 to 4 weeks of starting treatment and showing the best results after, around 12 weeks of continuous usage.
Dosage Adjustments for Special Populations
Patients with Hepatic or Renal Impairment
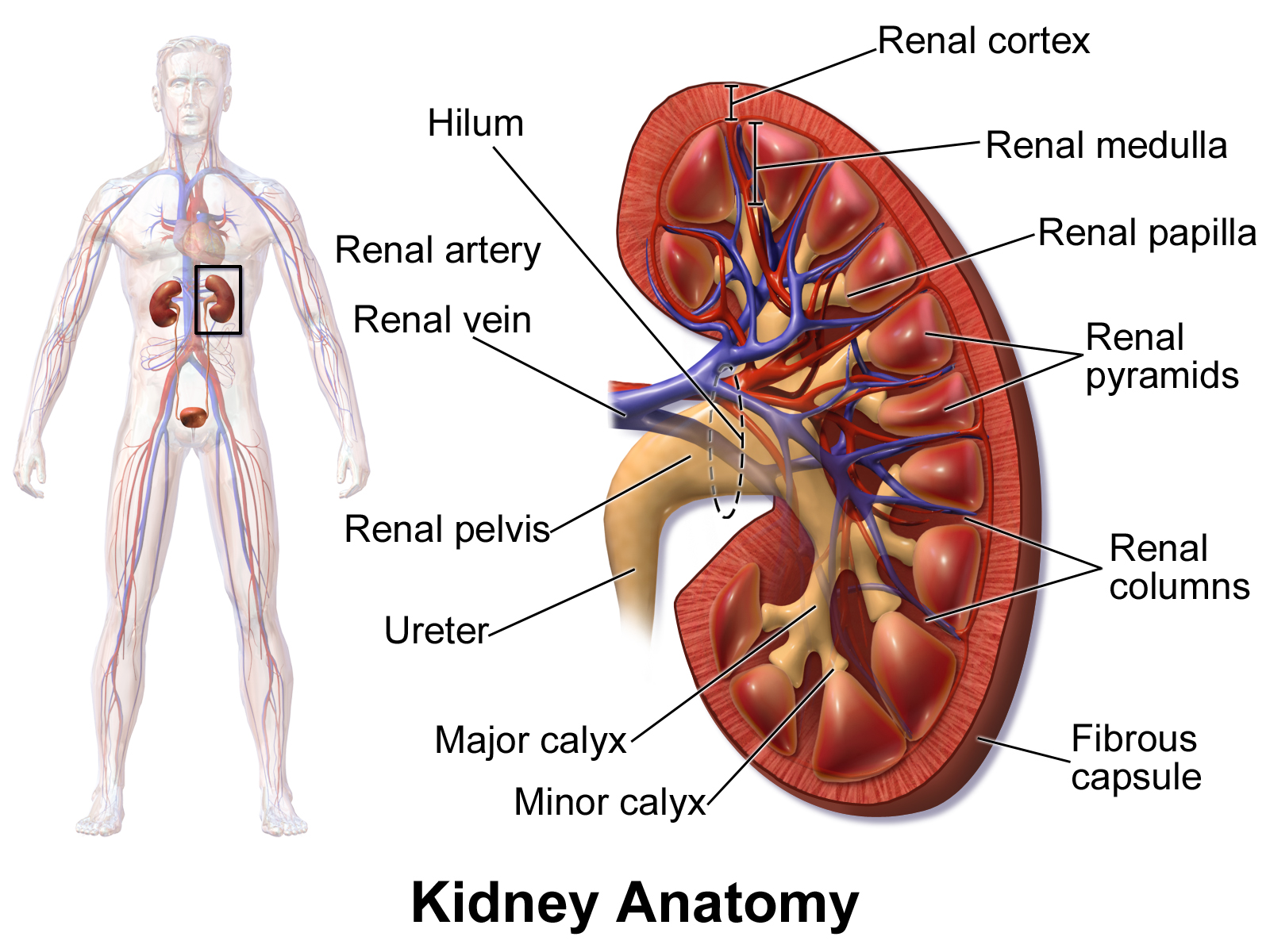
The processing of cilostazol, in the body mainly involves liver enzymes ( p450 isoforms) with kidney excretion playing a supporting role as well. For individuals, with liver or kidney issues;
Adjusting the dosage might be needed to avoid the build-up of the drug and potential harm to health.
- For individuals, with mild to liver issues; There's no need for changes in dosage; however it's best to keep a close watch and monitor the situation carefully.
- Severe liver damage may make it not recommended to use Cilostazol because it can affect how the drug is processed in the body and increase its presence, in the bloodstream.
- Renal dysfunction usually doesn't call for dosage adjustments, in mild to situations; however severe renal insufficiency (where CrCl is than 25 mL/min) requires a thorough evaluation of risks, versus benefits.
Elderly Patients
As people get older their bodies go through changes that affect how medications are processed in the liver and overall body function which means medication doses need to be adjusted for elderly individuals to avoid any reactions or side effects, like low blood pressure or rapid heartbeat caused by increased blood vessel dilation responses and any dose adjustments should be made according to how well each person can handle the medication.
Administration Guidelines
Best Time to Take Cilodoc for Maximum Efficacy
For the best results, from cilostazols effects to kick in fully and maintain their effectiveness throughout the day timed doses are recommended to be taken every 12 hours to keep plasma levels stable, for optimum vascular benefits.
Instructions Regarding Food Intake
The absorption of Cilostazol is greatly affected by consuming food with it. If taken along with a high-fat meal the amount of the drug that enters the bloodstream increases significantly, which could lead to a chance of experiencing side effects, like headaches and palpitations. To reduce these risks, it is advised to take Cilostazol; Remember to wait for at least half an hour before eating or wait for two hours after your meal. A glass of water is best to help with absorption.

Duration of Treatment and Expected Outcomes
When it comes to treating term conditions with medication, like cilostazol therapy you need patience and dedication to see real results over time. The treatment process is expected to show results, and it may take some time before noticeable improvements are seen. Relief of symptoms usually becomes noticeable after using the product for 2 to 4 weeks. Optimal progress, in treatment typically occurs around 12 to 16 weeks, resulting in improvement. For lasting effectiveness ; Consistent use might be necessary to maintain advantages and regular evaluation to determine ongoing therapeutic need.
Cilostazol Dose for Peripheral Arterial Disease
For signs of arterial disease, beyond intermittent claudication, treatment recommendations remain the standard (100 mg twice daily). Patients needing antiplatelet therapy along with it (like aspirin or clopidogrel), it's important to monitor them to prevent excessive bleeding or hemodynamic instability. Regular check ups and clinical evaluations are crucial to assess how well the treatment is working and make any necessary changes, to the dosages as needed. If there is no improvement noted within 3 to 6 months other treatment options can be explored.
Cilostazol Side Effects
Common Side Effects of Cilostazol
While Cilostazol is known for its effectiveness, in enhancing blood flow and decreasing platelet clumping it does come with a range of impacts. Many of these side effects are generally mild and temporary, often fading away as the body gets used to the medication. However these instances can impact how well a person sticks to their treatment plan and their overall comfort level while taking the medication.
Headache
Frequently mentioned in reports are the effects of cilostazol, due to its ability to widen blood vessels, causing headaches as a common outcome of this property's effect on the body's vasodilation process, which can result in elevated pressure inside the skull, appearing as a persistent throbbing or pulsating pain sensation. Patients might notice signs of discomfort such, as;
- Headaches, at the front or side of the head that get worse, with activity. Take some comfort from drinking water and using pain relievers available, without a prescription. As you use it more your body gets used to it. The effects become less intense, over time.

Diarrhea
Digestive issues, like diarrhea can happen because cilostazol speeds up movement through its effects, in the body's mechanism of action which may result in;
- Experiencing diarrhea after taking the medication.
- Experiencing mild, to moderate dehydration can be concerning if it persists for a while.
- Making short-term changes, to your diet can help relieve symptoms.

Palpitations
By increasing the levels of a compound called cyclic adenosine monophosphate (also known as cAMP), inside cells of the heart muscle cells cardiologists can make the heart pump harder and sometimes causing patients to feel a flutter, in their chest known as palpitations that they might mention during a doctors visit.
- Feeling a flutter, in the chest.
- At times my heart beats irregularly or quickly.
- An increased sensitivity to the rhythm of their heartbeat is noticeable, during moments of rest.
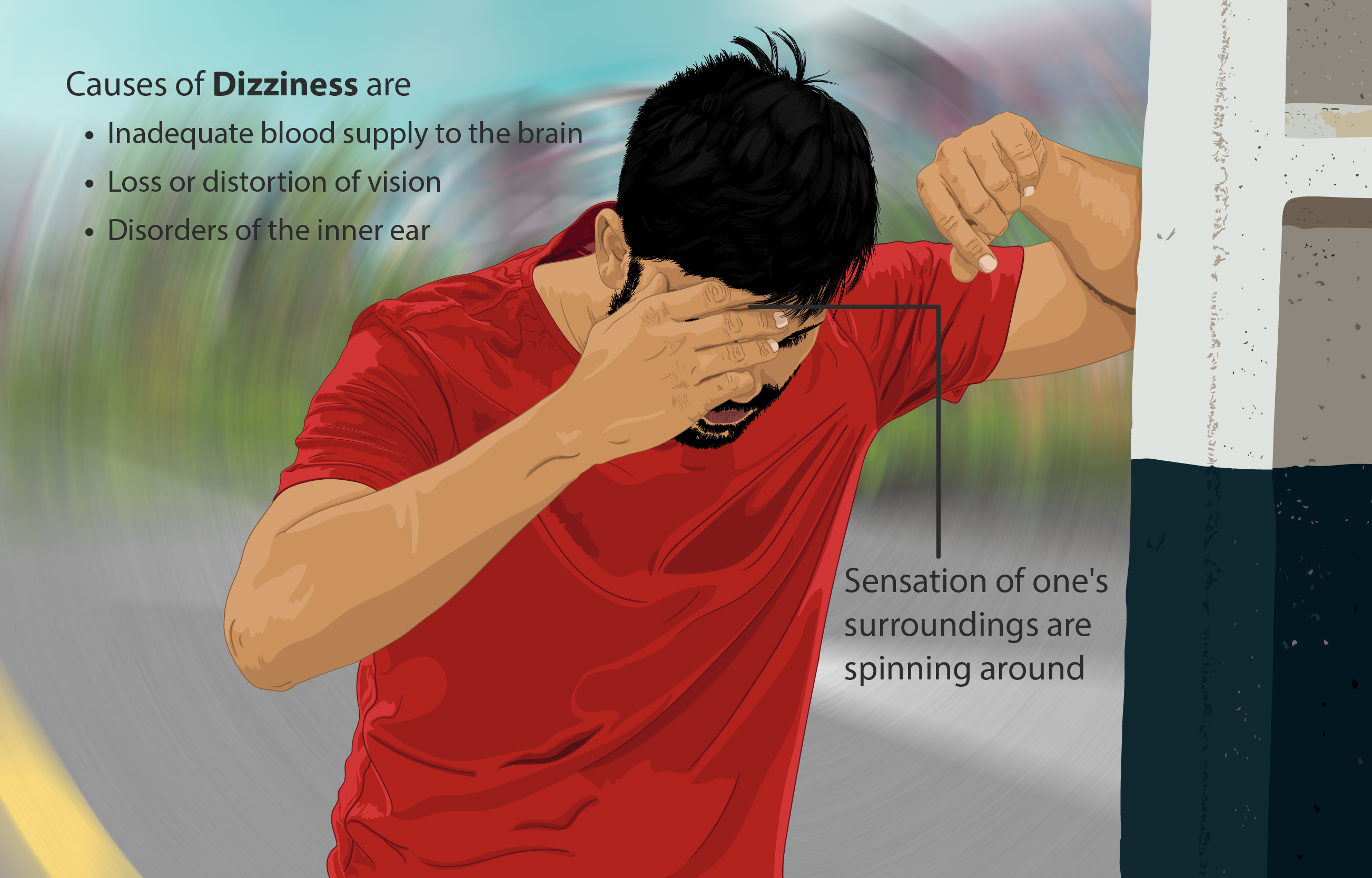
Dizziness
When cilostazol acts as a vasodilator, in the body it has the potential to reduce blood pressure levels which can sometimes result in orthostatic dizziness being experienced by individuals.
- Feeling dizzy when getting up quickly from sitting or lying down abruptly.
- Episodes of dizziness. A sensation of spinning.
- Symptoms are getting better with adjustments, in position.
Peripheral Edema
Excessive fluid buildup, in the limbs often manifests in the legs and ankles because of alterations, in blood vessel permeability leading to swelling known as peripheral edema.
- Swelling without pain, in the feet and ankles.
- Slight unease worsened by sitting or standing for periods of time.
- Enhancing recovery through raising the limb and utilizing compression therapy techniques.
Serious Side Effects and Adverse Reactions
Although rare, some negative impacts require attention because of their serious nature.
Bleeding Complications
When cilostazol is combined with antiplatelet medications, such as aspirin or clopidogrel it can raise the chances of bleeding by affecting how platelets clump together. Signs that bleeding may be too much include;
- Bruises easily and experiences longer bleeding from cuts is an occurrence for some people, with this condition.
- Passage; Hematuria refers to the presence of blood, in the urine while melena describes stools that're black and tarry.
- Severe cases may result in bleeding.

Tachycardia and Arrhythmias
People, with a risk of heart issues might experience heartbeats originating from the lower or upper chambers of the heart known as ventricular or supraventricular tachycardia, respectively. Symptoms may manifest as follows;
- Heart pounding fiercely at a rate surpassing 100 beats, per minute.
- Episodes of irregular heartbeat or missed heartbeats.
- In some situations, individuals may experience difficulty breathing or discomfort in the chest area.
Hypersensitivity Reactions
While uncommonly occurring. Allergic responses, to cilostazol may present as follows;
- Skin rash may cause itching or hives, on the skin.
- Swelling of the face due, to angioedema issues.
- Experiencing reactions that necessitate immediate emergency intervention.

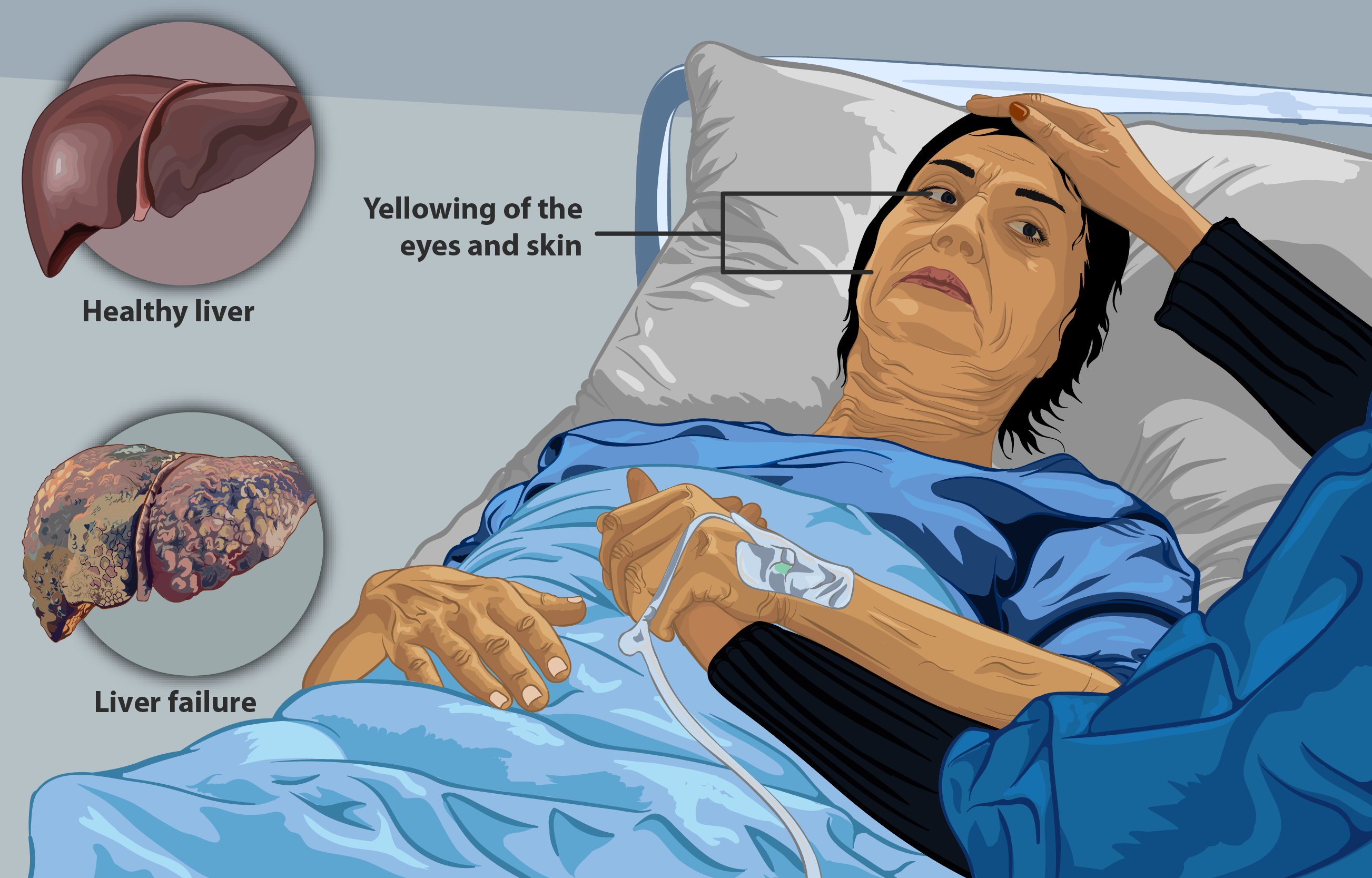
Liver Function Abnormalities
In some people, with conditions or circumstances Hepatic enzyme levels might increase, which could potentially affect the livers function adversely and indicate signs of liver toxicity such, as;
- Jaundice is indicated by the yellowing of the skin or the whites of the eyes (sclera).
- Feeling tired, for no reason and noticing dark colored urine in your body.
- Abnormal levels of liver enzymes were detected in the lab tests.
Cilostazol Side Effects in Vascular Conditions
Patients who already have issues might experience a risk of low blood pressure or increased heart rate due to cilostazol treatment, so healthcare providers need to watch out for excessive widening of blood vessels in people, with high blood pressure or heart problems.
Cilostazol Side Effects in Diabetes
People who have diabetes and especially those, with autonomic neuropathy might feel blood vessel dilation effects that can cause low blood pressure when standing up. Furthermore, cilostazol's effect on activity could affect the healing process of foot ulcers, in individuals.
Cilostazol Interactions
Major Drug Interactions
Anticoagulants and Antiplatelet Drugs
When cilostazol is combined with agents it shows anticoagulant effects that work together harmoniously.
- Warfarin poses a chance of causing bleeding, in the stomach and intercranial hemorrhage.
- Aspirin and Clopidogrel lead, to increased inhibition of platelets. May necessitate monitoring for signs of bleeding risks.
CYP3A4 and CYP2C19 Inhibitors and Inducers
Cilostazol's metabolism is greatly influenced by being a substrate of P450 enzymes.
- Certain substances, like Ketoconazole and Erythromycin can elevate the levels of cilostazol in the bloodstream, which may lead to intensified side effects.
- Inducers, like Rifampin and Carbamazepine can speed up metabolism. Decrease the effectiveness of treatment.
Calcium Channel Blockers and Beta-Blockers
When combined with blood pressure medications, like amlodipine or metoprolol there could be effects.
- Excessive widening of blood vessels leading to blood pressure.
- Rapid heart rate reflexes are especially common, in individuals, with compromised heart function.
Food and Alcohol Interactions
Impact of High-Fat Meals on Absorption
Indulging in meals, with content can greatly improve the absorption of cilostazol into the body. This can result in increased bioavailability of the medication.
- Increased levels of medication, in the bloodstream.
- There has been a rise, in reports of headaches and palpitations.
- To minimize these impacts of cilostazol on the body's system you should consume the medication 30 minutes before eating. Wait for 2 hours after finishing a meal.
Effects of Alcohol on Efficacy and Side Effects
Drinking alcohol can enhance vasodilation effects. Worsen blood pressure caused by cilostazol intake, which may lead to;
- Feeling more lightheaded and at a risk of fainting.
- Feeling more heartbeats racing because of the body's response.
- Patients should consider reducing their alcohol consumption to avoid interactions, with medications.
Contraindications for Cilodoc (Cilostazol)
Absolute Contraindications
Patients, with health conditions should avoid using Cilodoc (also known as Cilostazol) as it can lead to side effects that may harm their well being and safety.
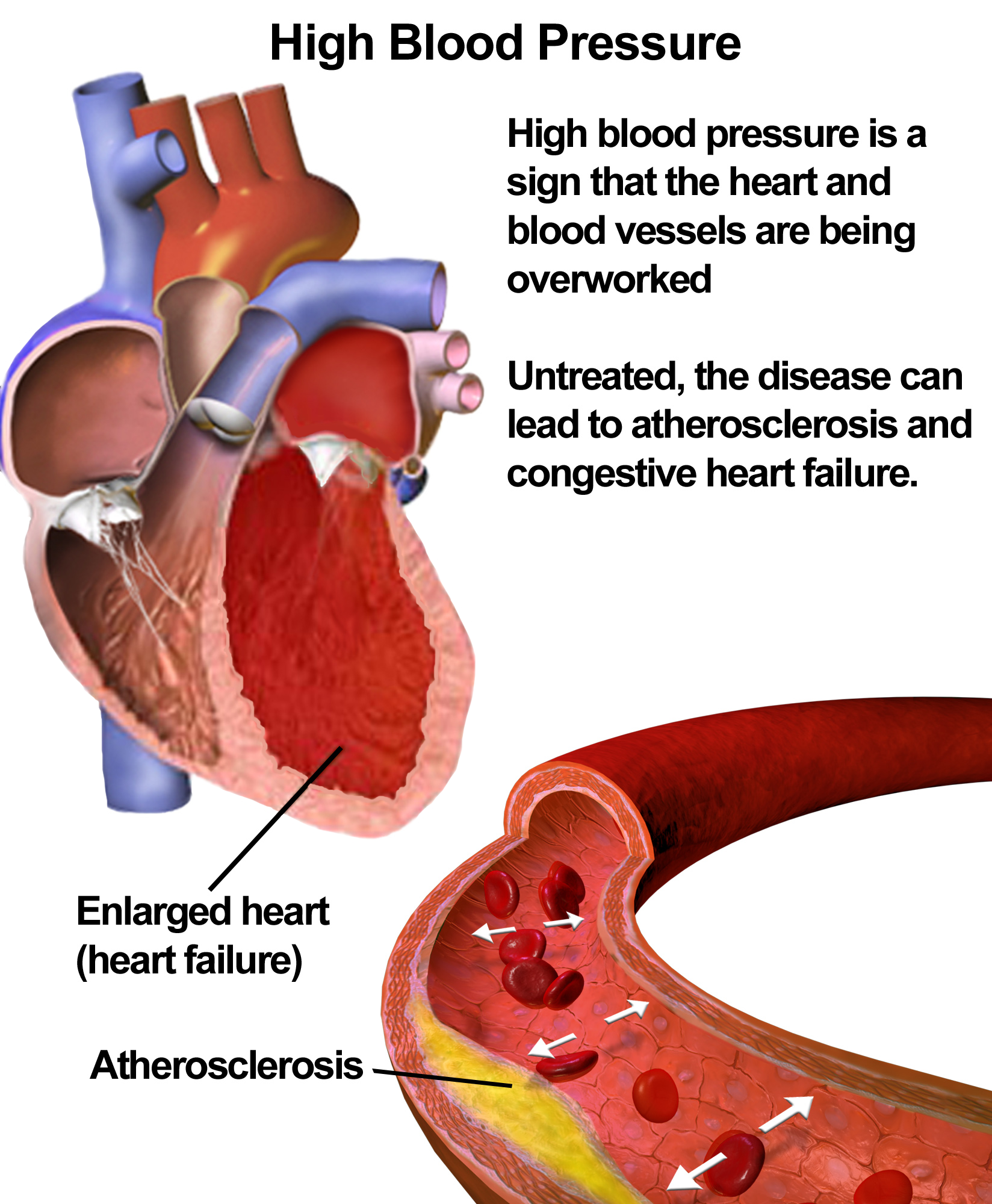
Patients with Severe Heart Failure
People who have congestive heart failure (CHF) should not be prescribed cilostazol as it can have an impact, on the hearts ability to pump effectively by increasing its workload through the inhibition of phosphodiesterase 4 (PDE4). This can result in;
- The heightened chance of heartbeats and unexpected cardiac arrest is a concern.
- The deterioration of the hearts ability to pump blood among individuals, with a decreased ejection fraction, in the ventricle.
- Worsening of accumulation and congestion, in the lungs.
Regulatory bodies, like the FDA and EMA, have clearly stated that cilostazol is not recommended for patients, with any form of heart failure (CH).
Uncontrolled Bleeding Disorders
Cilostazol should not be used in patients, with high-risk bleeding issues due, to its antiplatelet properties.
- Conditions, like ulcers or esophageal varices can cause bleeding.
- A previous incident of bleeding inside the skull has. Increasing suppression could lead to severe consequences.
- Severe drop, in platelet count, causing bleeding issues.
Hypersensitivity to Cilostazol or Excipients
It is important, for individuals who have previously experienced hypersensitivity reactions to cilostazol or any of its components to avoid using this medication as it could lead to a reaction characterized by symptoms such, as;
- Skin conditions, like hive like rashes or swelling known as urticaria and angioedema are manifestations to look out for.
- Difficulty, in breathing can involve conditions such, as bronchospasm or anaphylaxis.
- Immediate medical attention is needed for reactions.
Relative Contraindications
In some situations it's important to be careful when recommending treatment; close observation and evaluating risks, versus benefits are crucial, in instances.
Severe Hepatic or Renal Dysfunction
When it comes to cilostazol and how the body processes it in the liver through enzymes, like P450 ( CYP 34 and CYP 219) things can get more complicated for individuals, with liver issues.
- Changes in drug breakdown processes could result in levels of the substance circulating throughout the body.
- The likelihood of liver damage or heightened vasodilatory effects is heightened.
In cases of kidney impairment (CKS stage 4 or 5), it is important to be cautious, due, to the renal elimination of cilostazol metabolites.
- Prolonged drug effects can occur when active metabolites build up in the body over time.
- There is a possibility of a risk of bleeding because of difficulties, in excreting waste, from the body.
History of Arrhythmias
Caution should be taken when considering the impact of cilostazol, on the hearts activity in patients, with a history that includes;
- Excessive ectopic activity could potentially worsen arrhythmias in the presence of inhibition.
- Atrial fibrillation has the ability to increase activity.
- Patients who are taking medications that can prolong the QT interval may face an increased risk of QT prolongation.
Cilostazol Warnings and Precautions Before Using Cilodoc (Cilostazol)
Risk of Cardiovascular Events
While cilostazol has been shown to have effects on blood vessels' health, it has also been linked to a chance of severe heart-related issues in specific groups of people.
- The inotropic effects may lead to ventricular tachyarrhythmias in some cases.
- Individuals, with artery disease may experience a rise, in heart rate that could potentially cause harm.
- Worries, about the extended term risk of death are especially concerning for individuals, with existing heart problems.
Monitoring the heart health of patients, with existing issues is crucial, to their well-being and medical care needs.
Increased Bleeding Risk with Concurrent Anticoagulant Use
The way cilostazol works includes preventing platelet aggregation, especially when taken with anticoagulants, like;
- Warfarin may lead to INRs. Elevate the risk of unexpected bleeding episodes.
- DOAC medications pose a risk of causing bleeding, in the brain and digestive system compared to other treatments.
- Dual antiplatelet therapy (known as DAPT) requires monitoring due, to the combined effects of aspirin and clopidogrel working together synergistically.
It is recommended to check coagulation factors to reduce the chances of over anticoagulation.
Need for Periodic Monitoring of Blood Pressure and Liver Function
Since cilostazol can cause blood vessels to widen (vasodilation) it's important to check blood pressure levels. This is especially crucial, for the following situations;
- Patients, with blood pressure are susceptible to experiencing a drop, in blood pressure when changing positions, known as hypotension.
- Older people who might feel dizzy or faint.
Regular tests of liver function are necessary to identify any liver damage, over time with specific signs to watch out for including;
- High levels of alanine aminotransferase (ALT ). Aspartate aminotransferase (AST).
- Symptoms of liver issues, like yellowing skin or discomfort in the abdomen.
Importance of Adhering to Lifestyle Modifications
When cilostazol improves blood flow, in the limbs better when paired with lifestyle changes aimed at improving health and well being is suggested for patients to consider;
- Participate in guided physical activity sessions to enhance your ability to walk distances.
- Follow a diet that's good, for your heart by reducing your intake of foods, in saturated fats and processed carbohydrates.
- Quit smoking because using tobacco causes peripheral arterial disease.
- Ensure that you keep your blood sugar levels in check if you have diabetes.
By combining medication treatment with changes, in lifestyle habits and behaviors helps individuals attain results for their blood vessels and experience lasting relief, from symptoms over time.
Special Populations and Cilostazol Contraindications
Administration to Elderly Patients
Elderly individuals need attention when it comes to dosages because their bodies may respond differently to medications as they age. Even though cilostazol is a treatment, for peripheral arterial disease (PAD) it's crucial to be extra cautious when giving it to older patients.
- As people get older their blood vessels may become stiffer, which could make them more likely to experience high-blood pressure and dizziness when standing up.
- Increased Chance of Bleeding Risk, in Individuals; When older adults use both antiplatelet medications (such as aspirin and clopidogrel) along, with anticoagulants it heightens the likelihood of experiencing unexpected bleeding episodes.
- In individuals with reduced liver and kidney function medications may stay in the body longer, requiring changes or more frequent monitoring.
Starting treatment, with doses and adjusting as needed for tolerance could help reduce side effects in older patients who are frail or often take multiple medications.
Administration to Pregnant Women and Nursing Mothers
Pregnancy Category and Potential Fetal Risk
In the classification system, for pregnancy safety of medications known as Pregnancy Category C where cilostazol falls under it signifies that studies on animals have shown harm to the fetus while data from controlled studies are not enough to draw conclusions about its effects, on human fetuses yet.
- The strong vasodilatory effects of the substance could potentially impact the development of blood vessels, in the fetus.
- Worries, about the risk of bleeding due, to suppression have been raised.
It is advisable not to use cilostazol during pregnancy unless the benefits clearly outweigh the risks to the fetus due, to the lack of studies, on women.


Excretion in Breast Milk and Breastfeeding Recommendations
The full impact of excretion, into human breast milk is not fully known yet. However due to its binding to proteins and potential for overall effects it could present a hypothetical danger to breastfeeding babies. Guidelines, for mothers who are nursing include;
- If cilostazol therapy is required it is advised to refrain from breastfeeding during that time.
- Exploring treatment options that have documented safety records, for breastfeeding mothers.
- Opting for formula feeding as a substitute to avoid contact.
Cilostazol Nursing Considerations
Healthcare workers need to be careful when giving cilostazol to patients who are, at risk of complications or adverse effects.
- Keeping an eye out for any signs of bleeding like bruises or blood, in the urine and watching out for longer, than usual clotting times.
- Making sure that patients follow the advice to prevent worsening of side effects.
- Examining indicators such, as pulse rate and blood pressure to identify instances of rapid heart rhythms.
Administration to Children
The safety and effectiveness of Cilostazol, in children have not been clearly established because there are no clinical trials conducted on pediatric populations for this medication yet. It is not routinely recommended for use in children due to a lack of dosage guidelines and concerns regarding its suitability, for them.
- The immature autonomic regulation might lead to a risk of instability.
- Pharmacokinetics can vary unpredictably due, to differences in liver enzyme activity, during development.
- Long-term impacts on blood vessels, in developing individuals are not well documented.
Unless there is information, in the future to support it otherwise conclusively indicated by a specialist's oversight, cilostazol should not be recommended for individuals, below the age of 18.
Overdosage and Emergency Management
Symptoms of Overdose
Overindulging in cilostazol could lead to a medical emergency situation, where signs of an overdose may manifest as follows;
- Severe low blood pressure may occur due, to the widening of blood vessels and can cause faintness or a sudden drop, in circulation.
- High doses of the medication can lead to increased heart rate and irregular heartbeats such, as palpitations or abnormal rhythms, like fibrillation or ventricular tachycardia.
- Experiencing gastrointestinal discomfort may happen if you overdose on this medication as it could lead to feelings of nausea and vomiting accompanied by cramping caused by much PDE 4 inhibition.
Immediate First-Aid Measures
In the event of an overdose situation the primary goal should be to stabilize the neurological functions swiftly. Initial steps, for aid should encompass;
- Position the patient on their back, with the legs raised to address blood pressure concerns.
- Giving activated charcoal is recommended if the ingestion happened within one to two hours.
- Maintaining the openness of the air passage when consciousness is impaired.
Medical Interventions and Supportive Care
When dealing with an overdose of cilostazol in a hospital setting medical professionals employ measures to tackle complications.
- Fluid resuscitation involves administering solutions, like normal saline, to replenish intravascular volume.
- In case persistent low blood pressure is not responding to treatment and remains a challenge to manage effectively, doctors may need to consider using vasopressors, like norepinephrine.
- Continuous monitoring of the hearts activity, known as ECG monitoring is utilized to identify and address heart rhythms effectively.
There is no antidote, for an overdose of cilostazol, so the treatment mainly focuses on managing symptoms and providing support.
Storage and Handling Precautions
Optimal Storage Conditions
To maintain the effectiveness of cilostazol's properties it's crucial to store it under controlled conditions. The recommended settings, for storage encompass;
- Please keep the product at a temperature, between 15°C to 30°C (59°F to 86°F), avoiding exposure, to heat or cold environments.
- Ensure the tablets effectiveness by safeguarding it against moisture, which can lead to degradation and reduced efficacy.
- Keep the item in its packaging to protect it from sunlight and UV rays.
Shelf Life and Expiration Guidelines
Patients and healthcare providers are advised that cilostazol formulations can maintain their effectiveness, for a period of, up to 3 years if stored correctly.
- Make sure to check the expiration dates on your medication and dispose of any that have expired.
- It's best not to keep tablets in places with a lot of moisture, like bathrooms.
- Avoid using tablets that seem to have changed color or texture and appear to be crumbling.
Proper Disposal of Expired or Unused Medication
Properly disposing of cilostazol is crucial to avoid consumption and environmental harm. Here are some suggested ways to dispose of it safely;
- Make use of the drug return programs provided by pharmacies or government entities.
- Disposing of tablets by mixing them with materials, like coffee grounds or cat litter before throwing them in the household garbage bin.
- To prevent water contamination, it's best to refrain from flushing things down toilets or sinks.
Following the storage and disposal protocols is crucial, to guaranteeing the safety and effectiveness of medications while also being environmentally conscious.
Cilodoc, Cilostazol FAQ
- What is Cilostazol used for?
- Is Cilostazol a blood thinner?
- What is Cilostazol?
- Why is Cilostazol contraindicated in heart failure?
- Do Cilostazol side effects go away?
- Best time to take Cilostazol?
- How long does Cilostazol stay in your system?
- What are Cilostazol used for?
- What are Cilostazol pills used for?
- Are Clopidogrel and Cilostazol the same?
- Can Cilostazol cause bleeding?
- Can Cilostazol be crushed?
- Can Cilostazol lower blood pressure?
- Can Cilostazol and Clopidogrel be taken together?
- Can Cilostazol be cut in half?
- How Cilostazol works?
- Cilostazol how to take?
- Cilostazol how does it work?
- Cilostazol how long to work?
- Chat Cilostazol used for?
- Cilostazol what class of drug?
- Cilostazol what type of drug?
- Cilostazol what does it do?
- Chat is Cilostazol used to treat?
- Cilostazol when to take?
- Cilostazol when to stop before surgery?
- Cilostazol when to stop?
- When taking Cilostazol should avoid?
- When should Cilostazol be taken?
- Cilostazol where to buy?
- Cilostazol which group of drug?
- Cilostazol which class of drug?
- Why Cilostazol is contraindicated in heart failure?
- Why take Cilostazol on an empty stomach?
- Why take Cilostazol?
What is Cilostazol used for?
People mainly use cilostazol to address claudication—a condition resulting from blood circulation in the legs that causes pain when walking by enhancing blood flow and enabling individuals to walk farther without experiencing discomfort.
Is Cilostazol a blood thinner?
Cilostazol isn't considered a blood thinner; of affecting the bloods ability to clot like blood thinners such, as warfarin or aspirin do it works by inhibiting platelet aggregation and enhancing blood flow.
What is Cilostazol?
Cilozastol is a medicine that is taken to help with claudication by widening blood vessels and stopping blood platelets from clumping to increase blood flow and ease leg pain when walking.
Why is Cilostazol contraindicated in heart failure?
Patients, with heart failure should avoid taking Cilostazol as it can worsen symptoms by putting strain on the heart and potentially making the condition more severe through its effects, on blood vessels and heart function.
Do Cilostazol side effects go away?
Some of the side effects of taking Cilostazol like headaches or diarrhea could lessen as your body gets used to the medication.. If these side effects continue or worsen significantly it's essential to seek advice, from a healthcare professional.
Best time to take Cilostazol?
Cilostazol is typically taken twice a day, 30 minutes before breakfast and dinner, to maximize absorption and minimize the risk of gastrointestinal issues. It's important to take it consistently at the same times each day.
How long does Cilostazol stay in your system?
The effects of cilostazol last, for 11 hours on average. It typically takes 2 to 3 days for the medication to fully leave your body after you stop taking it. Factors such, as liver function can influence how long it takes for cilostazol to be eliminated from your system.
What are Cilostazol used for?
The main purpose of cilosotazol is to help individuals with claudication arising from artery disease by enhancing their walking ability and easing discomfort through enhanced blood circulation to the legs.
What are Cilostazol pills used for?
Pills containing cilosazol are prescribed to help with claudication by reducing leg pain during exercise, through blood flow and stopping blood platelets from clumping together.
Are Clopidogrel and Cilostazol the same?
Clopidogrel and Cilostazol are not identical; Clopidogrel helps lower the chances of stroke and heart attack, as an antiplatelet drug whereas Cilostazol's specifically for alleviating leg pain caused by circulation, in the body with distinct ways of functioning.
Can Cilostazol cause bleeding?
Although Cilostazol doesn't thin the blood itself it may raise the chance of bleeding because of how it affects platelet aggregation.This risk could be higher if combined with blood thinning drugs.
Can Cilostazol be crushed?
It is important not to crush or break Cilostazol tablets as it can affect the extended release formulation and may lead to absorption of the medication or possible side effects. Follow the prescribed instructions by taking the tablets whole.
Can Cilostazol lower blood pressure?
Although cilostazols main purpose is not to lower blood pressure and it is primarily known for its vasodilatory properties; there have been observations suggesting that it may have an effect, on blood pressure regulation in some cases which could be a concern for individuals, with pre existing low blood pressure conditions.
Can Cilostazol and Clopidogrel be taken together?
Doctors sometimes prescribe Cilostazol and Clopidogrel together because they work well together in improving blood flow and preventing platelet clumping in some situations.However care should be taken when using these medications simultaneously as it could potentially raise the chances of bleeding and ought to be managed under guidance.
Can Cilostazol be cut in half?
It is not recommended to split Cilostazol tablets in half because they are designed to release the medication over time and cutting them may interfere with how the drug works in the body.
How Cilostazol works?
When you take cilosazol it helps relax blood vessels and stops platelets from clumping together by blocking an enzyme called phosphodiesterase III. This can improve blood flow and ease symptoms of claudication.
Cilostazol how to take?
Patients usually take cilostazol twice half an hour before eating meals with a glass of water. Without crushing or chewing it to ensure it works effectively.
Cilostazol how does it work?
To alleviate the discomfort linked to claudication, in the legs Cilastozol boosts blood circulation by preventing platelet clustering and stimulating vasodilation to enhance blood flow while walking.
Cilostazol how long to work?
Usually it takes about 2 to 4 weeks for cil ostazol to show results in improving walking distance and reducing leg pain caused by claudication; however the full therapeutic effect might be experienced after, around 12 weeks of use.
Chat Cilostazol used for?
Cilozatol is prescribed for treating claudication—a condition that leads to leg pain caused by blood flow, in connection, with peripheral artery disease—by enhancing walking ability and alleviating leg discomfort during exercise.
Cilostazol what class of drug?
Cilostazol is categorized as one of the medications falling under the group of phosphodiesterase inhibitors that function by blocking the enzyme phosphodiesterase III to widen blood vessels and enhance blood circulation.
Cilostazol what type of drug?
Used as a medication, for patients with artery disease (PAD) cilostazol functions as both an antiplatelet and vasodilator agent, by inhibiting platelet aggregation and expanding blood vessels to enhance blood flow.
Cilostazol what does it do?
Improving circulation, in the legs cilostazol widens blood vessels. Prevents blood clots, which helps alleviate pain and enhances mobility for individuals, with claudication.
Chat is Cilostazol used to treat?
This medication called cilosazol is prescribed for claudication. A condition where pain, in the legs happens while walking due, to circulation.It aids in lessening this discomfort. Enables individuals to walk distances.
Cilostazol when to take?
Take Cilostazol two times a day. Once, before breakfast and before dinner 30 minutes ahead of time on an empty stomach, for best absorption and results.
Cilostazol when to stop before surgery?
It's important to pause taking Cilostazol for a minimum of 5 days before undergoing surgery to lower the chance of bleeding caused by its impact, on platelet aggregation processes. Make sure to adhere to the recommendations given by your healthcare provider regarding when to stop taking it.
Cilostazol when to stop?
If you encounter side effects, like bleeding or heart issues while taking cilostazol or if your doctor advises stopping the treatment due, to other health issues suspend the medication immediately.
When taking Cilostazol should avoid?
When you are, on Cilostazol medication it is important to consult your doctor before taking any blood thinning medications as it can elevate the chances of bleeding occurringnt. Don't consume grapefruits or grapefruit juice as they might reduce the efficacy of the drug.
When should Cilostazol be taken?
You should take cilostazol daily. Before breakfast and then again, before dinner. For better absorption and fewer stomach related side effects.
Cilostazol where to buy?
You can purchase Cilostazol at pharmacies or online, with a prescription from either option and, through online pharmacy services that ask for a valid prescription.
Cilostazol which group of drug?
The medication cilostazol is classified as a type of drug called phosphodiesterase III inhibitors, which are used to enhance blood circulation and alleviate symptoms linked to blood flow, in the body.
Cilostazol which class of drug?
Cilostazol falls under the category of phosphodiesterase inhibitors as it targets phosphodiesterase III – an enzyme that plays a role, in regulating blood vessel widening and platelet clumping.
Why Cilostazol is contraindicated in heart failure?
Using cilostazol in patients, with heart failure is not recommended as it may worsen the condition by putting strain on the heart and causing an increase in heart failure symptoms well, as possible complications.
Why take Cilostazol on an empty stomach?
Its recommended to take cilostazol on a stomach since food can lower its absorption rate and diminish its effectiveness; ideally take it 30 minutes before meals, for the absorption results.
Why take Cilostazol?
Individuals take cil osta zol to alleviate the signs of claudication, like leg discomfort due to blood flow, in the bodys peripheral arteries; it enhances mobility and enhances the overall quality of life for those affected by peripheral artery disease.



















