Cordarone Injection
- Introduction
- Composition
- Cordarone injection uses
- Mechanism of Action: How Cordarone Injection Works
- Amiodarone dosage guide and Administration
- Storage Guidelines
- Side effects of cordarone injection
- Amiodarone drug interactions
- Warnings and Contraindications
- Careful Administration
- Administration to Special Populations
- Overdosage
- Handling Precautions
- Important Precautions
Introduction
Overview of Cordarone Injection
Cordarone Injection is a medicine mainly used to treat heart rhythm issues. It administers Amiodarone directly into the bloodstream for quick therapeutic results.
Historical Background and Development
Cordarone was first developed in the 1960s as a response to challenging cases of arrhythmias that were difficult to treat at the time. Through testing and trials over the years it has emerged as a player, in managing arrhythmias worldwide.
Importance in Modern Medical Practice
In todays cardiac care environments Cordarone Injection plays a role. It helps manage heart rhythm irregularities and supports patients facing serious heart issues.
Composition
Active Ingredient: Amiodarone Hydrochloride
The primary component, Amiodarone hydrochloride, exerts its therapeutic effects by modulating cardiac electrical activity, ensuring stable heart rhythms.
Inactive Ingredients and Excipients
Cordarone's composition comprises solvents and stabilizers that guarantee its durability and effectiveness throughout its shelf life. These additional ingredients also help preserve its benefits over time.
Formulation Details and Concentration
The injection is usually found in vials, with 50 mg/mL of Amiodarone hydrochloride for use, under medical monitoring.
Amiodarone vs adenosine
Adenosine and amiodarone help control heart rhythms in settings like hospitals and clinics. In practice settings where doctors treat episodes of heartbeats originating in the heart's upper chambers, known as paroxysmal supraventricular tachycardia, or PSVT for short, is often managed using adenosine. Amiodarone is another medication that can be used to address types of heart rhythms, including supraventricular and ventricular tachycardia and irregular heartbeats, like premature beats and atrial fibrillation.
Dronedarone vs amiodarone
It developed as a variation of amiodarone. Without the iodine component, it lowers the risk of harmful side effects. Dronedarone is considered an option compared to amiodarone.
Multaq vs amiodarone
Multaq or dronedarone is a revised form of amiodarone that does not contain iodine and offers the benefit of having side effects, like thyroid and lung toxicity, compared to amiodarone.
Amiodarone vs cardizem
Amiodarone is prescribed for heart rhythm issues. Due to its similarity to thyroid hormones, it can have side effects linked to the thyroid and lungs. Cardizem is utilized in managing chest pain resulting from blood flow to the heart.
Cordarone injection uses
Approved Medical Indications
- Management of ventricular arrhythmias
- Control of atrial fibrillation and flutter
- Treatment of supraventricular tachycardia
Amiodarone for afib
Off-Label Uses
- Prevention of sudden cardiac death
- Post-cardiac surgery arrhythmia control
- Management of refractory heart conditions resistant to other therapies
Amiodarone bradycardia
Amiodarone, prescribed for cardiac conditions, including dysrhythmia, is associated with bradycardia.
Mechanism of Action: How Cordarone Injection Works
Pharmacodynamics and Electrophysiological Effects
Amiodarone changes the characteristics of the heart to control heartbeats by prolonging the time for which the heart's cells are stimulated.
Impact on Cardiac Ion Channels
The medication impacts potassium and sodium channels as calcium channels to prevent irregular heart activity by affecting the process of heart muscle contraction and relaxation essential for treating arrhythmias.
Antiarrhythmic Classifications and Implications
Amiodarone stands out as a Class III antiarrhythmic due to its ability to incorporate characteristics of other classes of medications and boost its effectiveness for treatment purposes.
Amiodarone half life
The prescribing information for amiodarone states that the average time it takes for the drug to be eliminated in the bloodstream is 58 days (with a range of 15 to 142 days). Additionally, the active metabolite of amiodarone has a life ranging between 14 and 75 days.
Amiodarone dosage guide and Administration
Amiodarone dose
A common starting dose is 150 milligrams given through an IV over a period of 1o minutes. Then adjusted with an infusion based on the patient's requirements.
Maximum dose of amiodarone in 24 hours
For adults initially administer 5 milligrams, per kilogram through infusion over a duration of 20 to 120 minutes; can repeat infusion up to a total of 1200 milligrams ( 15 milligrams, per kilogram ) within a span of 24 hours.
Methods of Administration
- Intravenous Bolus: Rapid delivery in acute settings
- Continuous Infusion Protocols: Sustained administration for prolonged effect
Adjustments for Special Populations
Elderly patients and individuals with liver or kidney issues, need to have their dosages adjusted to avoid any effects.
Storage Guidelines
Optimal Storage Conditions
Please keep the item in an area with regulated room temperatures between 15 and 30 degrees Celsius. Make sure to shield it from light and freezing conditions.
Shelf Life and Stability Considerations
Make sure to check the expiry dates carefully to guarantee effectiveness and safety.
Handling During Emergencies
In situations make sure the remedy is transparent and devoid of any particles, before giving it.
Side effects of cordarone injection
Common Side Effects

Amiodarone blue skin
Amiodarone is recognized for triggering skin and overall side effects, with photosensitivity being the skin-related issue observed as a blue-gray discoloration on sun-exposed body areas.
Severe Adverse Effects
- Pulmonary toxicity, including fibrosis
- Thyroid dysfunction (hyperthyroidism or hypothyroidism)
- Elevated hepatic enzymes indicating potential liver injury
Amiodarone drug interactions
Interaction with Other Antiarrhythmic Drugs
Be cautious when using Amiodarone with antiarrhythmics as it can heighten the chances of occurring, necessitating careful monitoring.
Effects with Anticoagulants and Antiplatelet Agents
Amiodarone enhances the impact of blood thinners such as warfarin, which may require changes in dosage.
Amiodarone and warfarin
Amiodarone slows down the breakdown of warfarin in the body. When used together with warfarin treatment, it can lead to bleeding.
Combined Use with Beta-Blockers and Calcium Channel Blockers
Excessive synergy between factors could result in bradycardia or heart blockage.

Warnings and Contraindications
Situations Requiring Caution
- Severe sinus node dysfunction
- Pre-existing hypotension or bradycardia
Individuals with Known Hypersensitivity to Iodine
Amiodarone includes iodine, which can be risky for individuals with iodine allergies.
Absolute Contraindications
- Concurrent use with certain drugs like MAO inhibitors
- Patients with advanced atrioventricular block without a pacemaker

Amiodarone toxicity
The primary challenges associated with prolonged usage of amiodarone include lung issues such as toxicity and thyroid and liver problems.
Amiodarone toxicity symptoms
Symptoms may manifest as worsening shortness of breath over time, dry cough, fatigue, and sharp chest pain when breathing. Bilateral crackles could be detected during an examination.
Amiodarone and thyroid
Amiodarone can cause side effects such as thyroid problems (hypo- and hyperthyroidism) due to its iodine levels and direct harmful impact on the thyroid gland.
Amiodarone nursing considerations
Before giving any medication, it's important to check the patient's blood pressure and pulse rate at the heart's apex and use a heart monitor for those on amiodarone treatment. It's advisable to have a baseline chest X-ray and pulmonary function test done prior to starting treatment.
Careful Administration
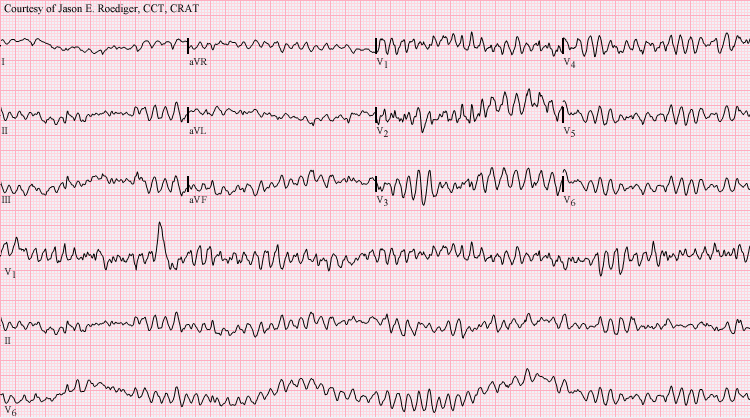
Monitoring Requirements During Treatment
It is crucial to consistently monitor patients when giving Cordarone Injection including electrocardiograms (ECGs). It is essential to conduct checks of liver and thyroid function to detect any organ specific toxicity early.
Adjustments for Renal or Hepatic Impairment
Individuals, with impaired kidney or liver function need personalized dosages. Due to elimination rates in these groups, it is important to adjust doses to prevent harmful effects and build-up of toxins.
Management of Side Effects During Prolonged Use
Side effects such as photosensitivity and pulmonary fibrosis must be actively managed during long-term therapy. Educating patients on preventive measures, like avoiding excessive sunlight exposure, can mitigate risks significantly.
Administration to Special Populations
Elderly Patients
Dosage Considerations for Age-Related Changes
As people grow older, their bodies change, affecting how medications work differently in them than in individuals do. This is known as pharmacokinetics due to age-related physiological changes observed in elderly patients. To ensure the well-being of patients, it is recommended to start with doses of medication and gradually increase them over time to avoid putting too much pressure on their heart and liver functions.
Risks of Prolonged Administration in Older Adults
Prolonged administration in this demographic elevates the risk of arrhythmias, hypotension, and cumulative organ toxicity. Frequent assessments and cautious dose adjustments are crucial for safe therapy.
Pregnant Women and Nursing Mothers
Potential Risks to Fetal Development
The Cordarone Injection falls into the category of medications that carry a risk during pregnancy because it can pass through the placenta and lead to issues like hypothyroidism and slowed growth; it's advisable to use it only if the benefits outweigh the risks.
Transfer to Breast Milk and Lactation Advice
Amiodarone and its metabolites are excreted into breast milk, warranting caution. Nursing mothers are advised to discontinue breastfeeding or explore alternative therapies.

Children and Adolescents
Safety Profile and Dosage Recommendations for Pediatric Use
In pediatrics Cordarone Injection is rarely, usually, for serious heart rhythm problems that don't respond to standard treatments. It's essential to calculate the dosage based on the childs weight carefully to prevent any risk of overdose or harmful effects.
Overdosage
Symptoms of Cordarone Injection Overdose
An overdose could show up as a heart rate or low blood pressure. It might lead to irregular, severe heartbeats as well. Neurological signs, like shaking and disorientation could also appear in situations.
Immediate Management and Interventions
The initial action to take is to stop the infusion process when needed in situations as a priority step, followed by providing necessary supportive treatments like administering fluids intravenously and using vasopressors to help stabilize blood pressure and heart rate levels accordingly if required for the patient well being and comfort. Supporting protocols such as cardiac life support should be promptly implemented if indicated or necessary, in such cases.
Long-Term Complications and Follow-Up Care
Patients who are recovering from an overdose need to be closely monitored for any hepatic issues that may arise in the term, and it is important for them to have regular checkups with both cardiology and internal medicine specialists to ensure a complete recovery journey.
Handling Precautions
Safe Preparation and Administration Protocols
Make sure to prepare Cordarone Injection in a setting to keep it effective and safe for use. Precision is key when measuring the dosage, and using equipment can help prevent mistakes when giving the injection.
Avoiding Contamination During Handling
In this setup, it's crucial to follow hygiene practices when handling devices and tools. Refrain from contact with any uncovered parts, and remember to use single-use syringes and gloves while getting things ready.
Disposal Guidelines for Unused Medication
Unused or expired Cordarone Injection should be disposed of according to hazardous waste disposal regulations to avoid exposure or environmental contamination.
Important Precautions
Pre-Treatment Assessments and Diagnostics
Perform evaluations that involve checking thyroid and liver function through tests, as well as conducting chest X-rays and ECGs, to identify any existing health issues and ensure a safer start to treatment.
Long-Term Monitoring for Organ-Specific Toxicity
It is important to conduct check ins to catch and address any negative effects at an early stage. Areas that need attention are the lungs,liver and thyroid function.
Patient Education on Recognizing Early Warning Signs
Patients should be informed about recognizing and reporting symptoms, like a prolonged cough or increased heart rhythm irregularities, promptly to minimize the chances of complications through communication.
Cordarone Injection FAQ
- What is the use of Cordarone injection?
- What is Cordarone used for?
- Why is Cordarone given?
- Where do you inject amiodarone?
- What happens if you push amiodarone too fast?
- What to avoid with Cordarone?
- How quickly does Cordarone work?
- Can amiodarone cause kidney problems?
- What is a cordarone injection used for?
- What is the major side effect of amiodarone?
- Why amiodarone is contraindicated during breastfeeding?
- Why amiodarone for afib?
- Why amiodarone in cardiac arrest?
- Amiodarone which drug?
- Where is amiodarone excreted?
- Where is amiodarone metabolized?
- What amiodarone treat?
- How amiodarone affect thyroid?
- How amiodarone works in cardiac arrest?
- How amiodarone cause hyperthyroidism?
- How amiodarone works on the heart?
- Can amiodarone cause dizziness?
- Can amiodarone lower blood pressure?
- Can amiodarone cause bradycardia?
- Can amiodarone cause hypotension?
- Are amiodarone and levophed compatible?
- Are amiodarone side effects reversible?
- Are amiodarone and dobutamine compatible?
- Are amiodarone and magnesium compatibility?
- Are amiodarone and heparin compatible?
What is the use of Cordarone injection?
The injection helps regulate your heartbeat.
What is Cordarone used for?
Amiodaron (trade name Cordarine) is a medication prescribed to treat heart rhythm disorders, such as fibrillation and tachycardia, as well as atrial fibrillation and flutter.
Why is Cordarone given?
Various forms of heartbeat, like fibrillation and tachycardia, are treated using this medication. It is classified as an antiarrhythmic drug and quickly helps your heart regain a stable and consistent rhythm.
Where do you inject amiodarone?
Amiodarone ought to be given via the central venous route.
What happens if you push amiodarone too fast?
It may lead to hypotension
What to avoid with Cordarone?
It's best to steer off grapefruits or grapefruit juice when you're on amiodarone medication.
How quickly does Cordarone work?
Amiodarone (brand names Cordarone and Paceone) is often prescribed as a medication. Its characteristic of being stored in the body's tissues rather than rapidly eliminated like many other drugs does set it apart. It may require several weeks to reach its peak efficacy and may persist in the body for weeks or even months after discontinuation of the last dosage.
Can amiodarone cause kidney problems?
Amiodarone can lead to kidney problems due to phospholipidosis.
What is a cordarone injection used for?
Cordarone Injection is a dosage prescribed for managing severe irregular heartbeat conditions like fibrillation and increased heart rate, known as tachycardia. Its function as a medication is to help stabilize your heartbeat to a consistent and normal rhythm.
What is the major side effect of amiodarone?
This medication has the potential to impact your heart's rhythm by inducing a condition known as QT prolongation, which could lead to faintness or severe side effects for individuals if you experience any signs of heart rhythm irregularities, like heartbeat or palpitations promptly inform your healthcare provider.
Why amiodarone is contraindicated during breastfeeding?
Amiodarone, a medication used to treat heart rhythms, may impact the thyroid function of breastfeeding babies.
Why amiodarone for afib?
It assists in maintaining a heart rhythm. It is particularly beneficial for individuals with preexisting heart conditions, such as heart failure.
Why amiodarone in cardiac arrest?
Amiodarone reduces the sensitivity of the heart tissue by extending the time it remains active. It stops any electrical signals from coming in to cause trouble.
Amiodarone which drug?
Amiodarone is a medication that belongs to the class and is used as an antiarrhythmic drug.
Where is amiodarone excreted?
The main route of elimination for Amiodarone is through the liver's metabolism and excretion via bile ducts.
Where is amiodarone metabolized?
Liver and gut
What amiodarone treat?
Amiodarone is prescribed for managing heart rhythm issues known as arrhythmias.
How amiodarone affect thyroid?
Amiodarone and its byproducts could potentially harm the cells in the thyroid gland directly and result in a type of thyroid inflammation known as thyroiditis.
How amiodarone works in cardiac arrest?
Upon receiving amiodarone, it works to ease the muscles along the walls of blood vessels, reduce peripheral vascular resistance (afterload), and slightly boost the cardiac index. When administered in this manner, it also reduces conduction to manage and prevent arrhythmias.
How amiodarone cause hyperthyroidism?
Amiodarone has the potential to induce hyperthyroidism, referred to as induced thyrotoxicosis (AIT), because of its iodine levels and its harmful impact on the thyroid gland.
How amiodarone works on the heart?
It directly affects the heart tissue. It helps to reduce the nerve signals in the heart.
Can amiodarone cause dizziness?
Amiodarone may lead to side effects such as nausea and vomiting as well as feelings of dizziness and constipation commonly experienced by individuals taking the medication.
Can amiodarone lower blood pressure?
Amiodarone also leads to the widening of blood vessels, which can cause a decrease in blood pressure.
Can amiodarone cause bradycardia?
Amiodarone has the potential to result in a decrease in heart rate, which is medically termed bradycardia.
Can amiodarone cause hypotension?
Administering amiodarone through an IV can lead to difficult-to-treat blood pressure issues.
Are amiodarone and levophed compatible?
There were no interactions between amiodarone and Levophed.
Are amiodarone side effects reversible?
Typical side effects of amiodarone may consist of feeling nauseous and vomiting or experiencing dizziness and constipation; if these symptoms become troublesome for you to handle, your healthcare provider might consider reducing your dosage levels. These side effects typically tend to get over time within a couple of weeks following that adjustment period.
Are amiodarone and dobutamine compatible?
Indeed. Amiodarone and dobutamine can be safely combined to address congestive heart failure.
Are amiodarone and magnesium compatibility?
Magnesium sulfate might speed up the elimination of Aminophylline, leading to a decrease in its blood levels and possibly reducing its effectiveness in the process. The chances of experiencing effects may rise when Aminodarone is used with Magnesium sulfate.
Are amiodarone and heparin compatible?
Amiodarone is a medication used to treat heart rhythms that may interact with other medications—both for the heart and for other conditions—and may also lead to blood thinning when combined with other blood-thinning agents, such as heparin.