Cephalothin, Cephaloridine, Injection
- Introduction to Cephalothin and Cephaloridine
- Composition and Formulation
- Uses of Cephalothin and Cephaloridine
- How Cephalothin and Cephaloridine Work
- Dosage and Administration
- Side Effects of Cephalothin and Cephaloridine
- Warnings and Contraindications
- Interactions with Other Medications
- Precautions for Special Populations
- Storage and Handling Precautions
- Overdose and Management
- Important Precautions for Safe Use
- Careful Administration Practices
Introduction to Cephalothin and Cephaloridine
Overview of Cephalothin and Cephaloridine
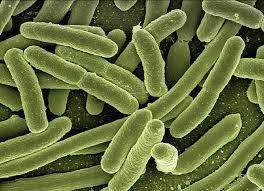
The antibiotics Cephalothin and Cephalordine belonging to the generation of cephalosporins are well known for treating a wide variety of bacterial infections when administered through injections. They play a role in fighting against both Gram-positive and specific Gram-negative bacteria strains.
Classification and Antibiotic Properties
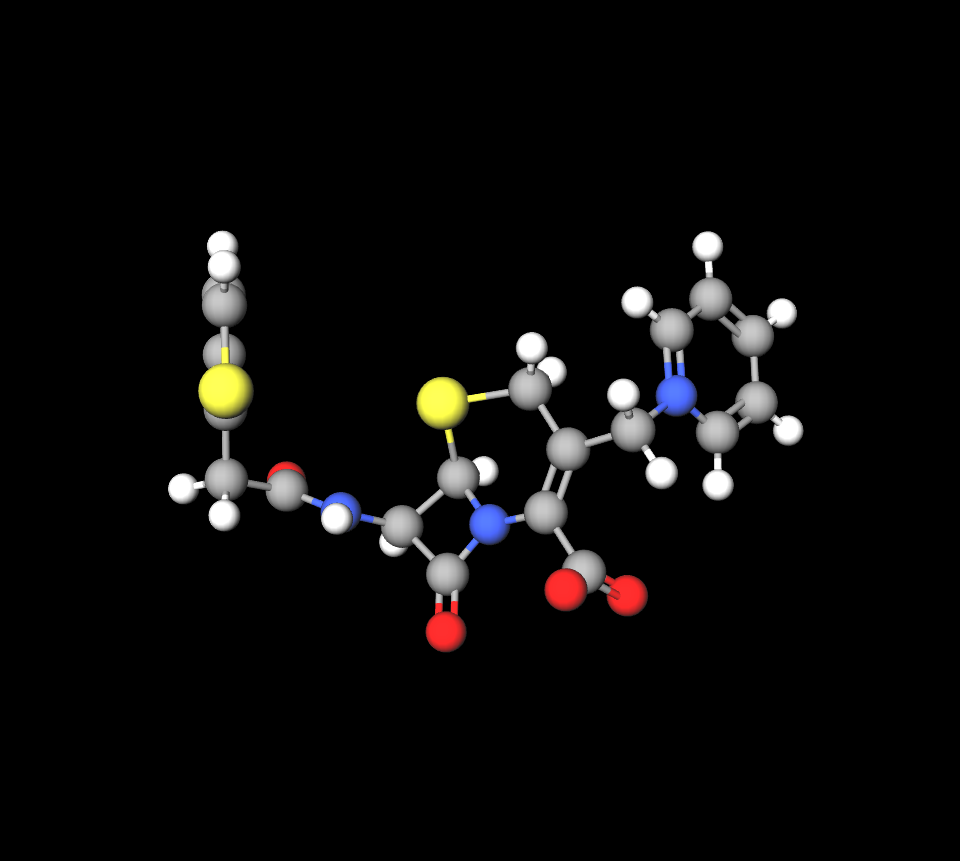
As members of the beta lactam group, Cephalothin and Cephaloridine work, by interfering with the formation of cell walls. This enables them to effectively combat both long-lasting infections due to their ability to kill bacteria.
Historical Development and FDA Approval
Introduced in the mid-20th century, Cephalothin and Cephaloridine gained FDA approval as revolutionary antibiotics, offering alternatives to penicillin derivatives for resistant strains.
Importance in Treating Bacterial Infections
These antibiotics play a role in the field of medicine by treating infections that vary from minor to case effectively and efficiently due to their specific targeting mechanism that helps prevent the spread of resistant strains.
Composition and Formulation
Active Ingredients: Cephalothin and Cephaloridine
The active ingredients are cephalosporin derivatives designed to maximize bacterial eradication while minimizing host toxicity.
Inactive Ingredients and Excipients
Crafted with stabilizing agents and additives to maintain the pH levels and prolong shelf life, these injections commonly contain sodium salts to improve solubility.
Cephalothin vs cephalexin
The functions of cephalexin and cephalothin are quite alike as they both belong to the first-generation cephalosporin group, with antibacterial activity levels compared to others in the category. They are mainly effective against Gram bacteria such as Streptococci, Staphylococci, and Enterococci.
Cephalothin vs cefazolin
The serum half life of cefazolin is compared to cephalothin. This enables it to retain concentrations in the bloodstream.
Available Forms and Strengths of the Injection
Both Cephalothin and Cephaloridine come in powder form that needs to be mixed with liquid before use; they have strengths ranging from 500 mg to 2 g per vial to meet medical needs.
Uses of Cephalothin and Cephaloridine
Primary Indications
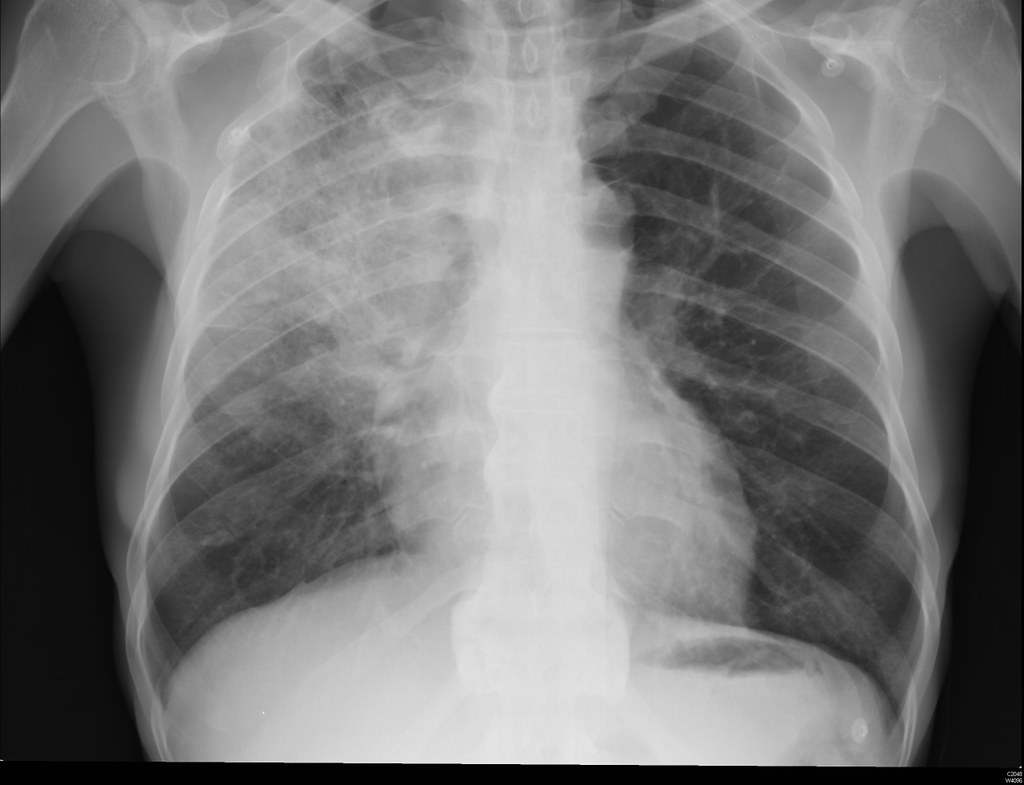
- Respiratory tract infections, including pneumonia and bronchitis.
- Urinary tract infections caused by susceptible bacteria.
- Skin and soft tissue infections, such as cellulitis and abscesses.
- Septicemia and bacteremia, especially in hospital settings.
Off-Label Uses
- Prophylactic use in surgical procedures to prevent post-operative infections.
- Treatment of multi-drug-resistant infections where other antibiotics have failed.
How Cephalothin and Cephaloridine Work
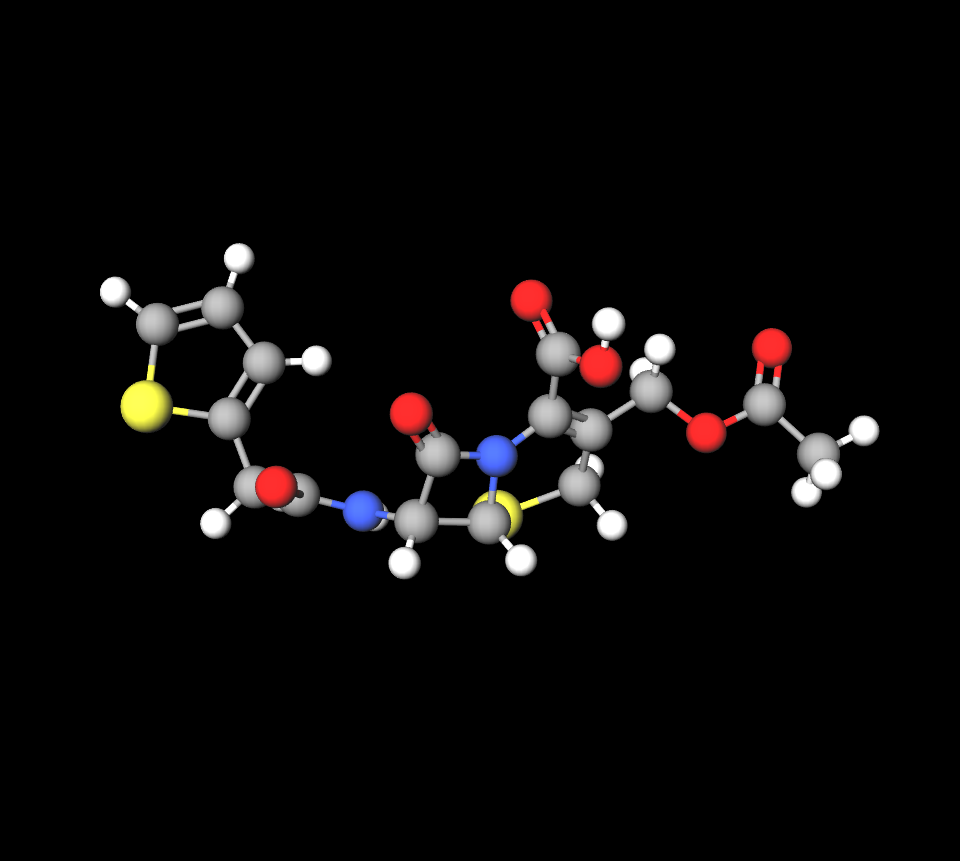
Mechanism of Action
These antibiotics stop transpeptidase enzymes that are important for building cell walls. This process causes the bacteria cells to become weaker and eventually break down.
Cephalothin method of action
The killing ability of cefalotin comes from blocking the production of cell walls by binding with penicillin-binding proteins (PBPs). PBPs are enzymes, for making peptidoglycan in the cell wall; hence stopping them hinders the formation of this important component.
Spectrum of Activity
The medications show effectiveness against bacteria that are Gram-positive, such as Staphylococcus aureus, and have moderate success in fighting certain types of Gram-negative bacteria like Escherichia coli.
Comparison of Efficacy
Cephalothin is noted for its superior activity against Gram-positive bacteria, whereas Cephaloridine offers enhanced penetration in certain tissue types, making them complementary in clinical use.
Dosage and Administration
Cephaloridine and Cephalothin dose
A dosage of 1-2 g every 6 hours is typical for severe infections. Adjustments are necessary based on severity and renal function.
Dosage Guidelines for Pediatric Use
Kids are typically advised to take between 50 to 100 milligrams per kilogram per day spread out over doses for their medication regimen; it's crucial to keep an eye to prevent any negative effects from occurring.
Administration Methods and Frequency
When given through a vein or a muscle injection method, it is chosen based on the type of infection present. Usually occurs every 6 to 12 hours as, per practice.
Adjustments for Renal and Hepatic Impairment
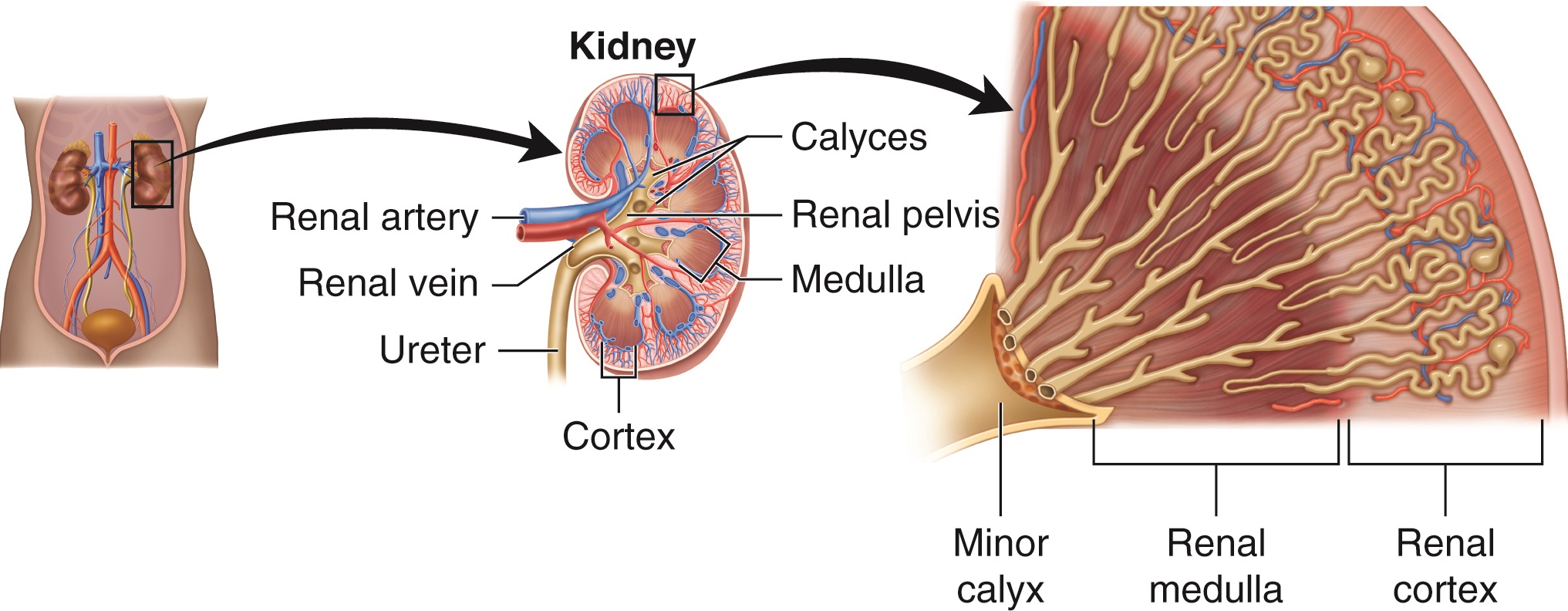
Patients with kidney issues may need to have gaps between doses to avoid the buildup of medication in their bodies and prevent side effects.
Side Effects of Cephalothin and Cephaloridine
Common Side Effects
- Mild gastrointestinal discomfort, including nausea and diarrhea.
- Localized pain or inflammation at the injection site.
- Occasional mild allergic reactions, such as rash or itching.

Rare but Serious Side Effects
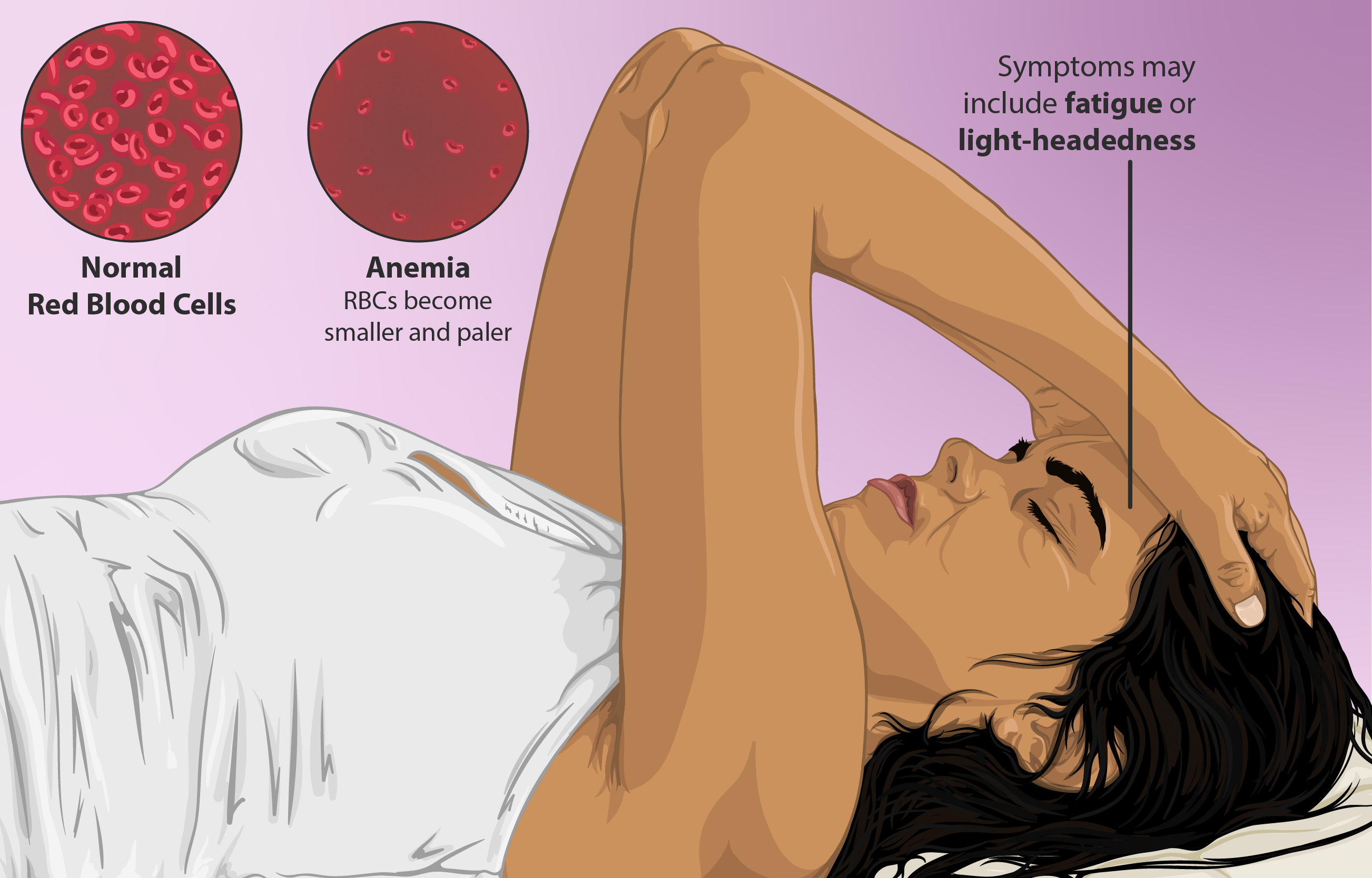
Side effects include anemia, thrombocytopenia, anaphylaxis, pseudomembranous colitis, and elevated hepatic enzymes.
Warnings and Contraindications
Absolute Contraindications
- Patients with a known hypersensitivity to cephalosporins.
- History of severe allergic reactions to beta-lactam antibiotics.
Conditions Requiring Caution
- Renal impairment, due to increased risk of nephrotoxicity.
- History of gastrointestinal diseases, such as colitis.
Interactions with Other Medications
Potential Drug Interactions
Cephalothin and Cephaloridine may interact with other medications, leading to amplified or diminished therapeutic effects. Identifying potential interactions is crucial to mitigate adverse outcomes.
Concomitant Use with Aminoglycosides
When aminoglycosides are used together with medications, there is a chance of kidney damage. This requires monitoring of kidney function. Making dosage changes thoughtfully.
Interaction with Anticoagulants
When taken together with blood thinners, like warfarin it can boost their blood thinning effects. Raise the chance of bleeding occurring. It is recommended to check coagulation levels to stay safe.
Impact on Laboratory Tests
Healthcare providers need to be aware that Cephalothin and Cephaloridine might affect the accuracy of laboratory tests, such as glucose or protein levels in urine, by causing positive outcomes. Recognizing this impact is crucial for selecting diagnostic approaches.
Precautions for Special Populations
Administration to Elderly Patients
The elderly are at increased risk of renal impairment, necessitating careful dosage adjustments. Renal function should be regularly assessed to minimize toxicity.
- Use the lowest effective dose to mitigate renal strain.
- Monitor for unusual side effects such as confusion or lethargy.
Administration to Pregnant Women and Nursing Mothers
These antibiotics demonstrate a favorable safety profile during pregnancy. However, their presence in breast milk warrants caution, as it could impact the nursing infant.
- Monitor infants for gastrointestinal disturbances or allergic reactions.
- Prescribe only when benefits outweigh potential risks.

Administration to Children
For pediatric patients, age-specific adjustments are critical. Regular monitoring can preempt potential adverse reactions, ensuring safe use.
- Administer doses based on weight and infection severity.
- Monitor for hypersensitivity or gastrointestinal symptoms.
Storage and Handling Precautions
Recommended Storage Conditions
Remember to keep the product in a place with stable room temperatures, around 20°C to 25°C, and shield it from sunlight or cold conditions.
Temperature and Light Sensitivity
Changes in temperature and exposure to light can reduce the effectiveness of the injection. It's important to store it to maintain its strength.
Shelf Life of the Injection
Make sure to follow the expiration date provided by the manufacturer and dispose of any solutions that have passed their expiration date to avoid any effects on treatment results.
Guidelines for Handling and Reconstitution
Prepare the injection by mixing it with diluent in an environment following a strict sterile procedure to ensure consistent concentration and avoid any risk of contamination.
Overdose and Management
Symptoms of Overdose
An overdose could result in issues such as seizures and gastrointestinal problems such as nausea or vomiting.

Emergency Treatment Protocols
Prompt and essential care is crucial in this situation; starting treatment quickly is key. For instance using antiemetics to address stomach discomfort.
Supportive Care and Monitoring
Patients need to be checked for their signs and kidney function to prevent any long-term harm and assist in their recovery process.
Dialysis in Severe Cases
In situations where the kidneys are not functioning enough to eliminate excess medication from the body efficiently; hemodialysis might be needed for patients who have kidney issues.

Important Precautions for Safe Use
Monitoring for Signs of Hypersensitivity Reactions
Regular assessment for allergic reactions is essential, especially during initial administration. Look for signs such as rash, hives, or breathing difficulty.
Regular Assessment of Renal Function
Regular checks on kidney function, help to keep the amount of medication in check to prevent kidney-related side effects.
Avoiding Prolonged Use to Prevent Superinfection
Extended therapy raises the chance of developing superinfections caused by bacteria; hence, it is advisable to restrict the usage to the period essential for achieving clinical progress.
Careful Administration Practices
Proper Techniques for Intramuscular and Intravenous Injection
Inject into the gluteal muscle for shots to reduce pain and administer intravenous injections slowly to prevent vein irritation.
Steps to Avoid Contamination During Preparation
Remember to use gloves and syringes when handling the vial to keep it sterile before using it; check that the seal is intact, and be careful not to touch the needles tip with your hands.
Importance of Adhering to Prescribed Doses
Make sure to follow the recommended dosage to avoid any results or harmful effects, and make sure to inform patients about the significance of finishing the treatment regimen.
Cephalothin, Cephaloridine, Injection FAQ
- What is cephalothin used for?
- What is cephalothin?
- How does cephalothin work?
- What is cephaloridine used for?
- What is cephalothin used for?
- What is the route of administration for cephaloridine?
- Which cephalosporins are nephrotoxic?
- What generation is cephaloridine?
- What are the side effects of cephalothin?
- Is cephalexin a safe drug?
- What bacteria does cephalothin treat?
- How does cephalothin work?
What is cephalothin used for?
Cefalotin is an antibiotic from the cephalosporin family that is commonly employed to combat infections in different areas of the body, including the urinary tract and respiratory system, alongside skin and bone infections.
What is cephalothin?
Cefalotin, also known as cephalothin, is a generation of cephalosporin with a wide range of antibiotic properties.
How does cephalothin work?
The reason why cefalotin is effective in killing bacteria is because it stops the formation of the cell wall by interacting with penicillin-binding proteins (PBPs). These PBPs are enzymes that play a role, in building peptidoglycan in the cell wall structure of bacteria.
What is cephaloridine used for?
It functions as an antibacterial medication. It belongs to the cephalosporin group—a semi-synthetic derivative known as a beta-lactam antibiotic allergen.
What is cephalothin used for?
Given during procedures and for addressing a variety of blood infections, it serves as both an antimicrobial substance and an antibacterial medication.
What is the route of administration for cephaloridine?
Upon injection, Cephaloridine is readily absorbed, while its absorption from the tract is limited.
Which cephalosporins are nephrotoxic?
The antibiotics cephalosporin, such as cephalothin, and cephalosporin, like cephalothin, are recognized for their ability to harm the kidneys. The extent of kidney damage caused by the variations of these antibiotics has not been fully understood yet.
What generation is cephaloridine?
This semisynthetic drug, called Cephalosporin, is effective against a range of bacteria as a first-generation cephalosporin.
What are the side effects of cephalothin?
Possible adverse reactions consist of red blood cell count (anemia), decreased platelet levels, severe allergic reactions (anaphylaxis), an intestinal condition characterized by inflammation and membrane formation (pseudomembranous colitis), digestive upset (diarrhea and nausea), and increased liver enzyme levels.
Is cephalexin a safe drug?
Most antibiotics, like cephalexin, have the potential to trigger a response that results in diarrhea.
What bacteria does cephalothin treat?
Staphylococcus and Streptococcus species.
How does cephalothin work?
Cefalotins ability to kill bacteria is due to its ability to block the synthesis of cell walls by binding to penicillin-binding proteins (PBPs).