1. Introduction to Lidocaine/Prilocaine
1.1 Overview of Lidocaine/Prilocaine
Lidocaine and Prilocaine are local anesthetics that are frequently combined in a single formulation to provide temporary numbness in a specific area of the skin. This combination is primarily used in medical settings to numb areas before procedures such as needle insertions, minor surgeries, or dermatological treatments. The synergy between these two anesthetics ensures longer-lasting effects and broader coverage.
1.2 Historical Development and Approval
The development of Lidocaine dates back to the 1940s when it was synthesized as a safer alternative to cocaine-based anesthetics. Prilocaine, introduced later, was formulated to complement the efficacy of Lidocaine while reducing certain side effects. In the 1980s, the combination of Lidocaine/Prilocaine received regulatory approval, revolutionizing minor surgical and dermatological procedures by providing reliable and safe anesthesia.
1.3 Purpose of Combining Lidocaine and Prilocaine
The combination of Lidocaine and Prilocaine is strategic. Lidocaine offers a rapid onset of action, while Prilocaine prolongs the anesthetic effect. Together, they create a formulation that provides comprehensive local anesthesia with fewer side effects than either agent used alone.
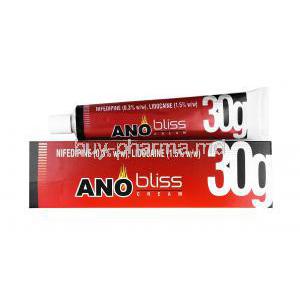
1.4 Common Brand Names and Formulations
Lidocaine/Prilocaine is marketed under several brand names, the most recognized being *EMLA* (Eutectic Mixture of Local Anesthetics). Available formulations include creams, gels, and transdermal patches, each tailored for specific medical uses.
2. Composition of Lidocaine/Prilocaine
2.1 Chemical Structure of Lidocaine
Lidocaine is an amide-type local anesthetic with the chemical structure C14H22N2O. Its hydrophobic properties allow it to efficiently penetrate nerve membranes, inhibiting pain signal transmission.
2.2 Chemical Structure of Prilocaine
Prilocaine, an amino amide, is structurally similar to Lidocaine but differs in its metabolism, allowing for a faster clearance in the body. Its chemical formula is C13H20N2O.
2.3 Mechanism of Action of Lidocaine
Lidocaine blocks sodium channels in neuronal membranes, preventing the initiation and propagation of action potentials. This results in the reversible loss of sensation in the targeted area.
2.4 Mechanism of Action of Prilocaine
Prilocaine works similarly by inhibiting sodium ion influx in nerves, but it is metabolized more quickly than Lidocaine, reducing the risk of systemic toxicity.
2.5 Available Dosage Forms (Creams, Gels, Patches)
Lidocaine/Prilocaine is available in multiple dosage forms, including creams (typically 2.5% Lidocaine and 2.5% Prilocaine), gels, and transdermal patches. These forms are designed to allow flexibility in administration, catering to both acute and prolonged pain management needs.
3. Uses of Lidocaine/Prilocaine
3.1 Approved Uses in Medical Practice
Lidocaine/Prilocaine is approved for use as a local anesthetic in several medical settings, including the numbing of the skin before venipuncture, minor surgery, or dermal treatments such as laser therapy.
3.2 Use in Dermatological Procedures
In dermatology, Lidocaine/Prilocaine is applied topically before procedures like mole removal, tattoo application, or laser hair removal to minimize patient discomfort.
3.3 Use in Dental Anesthesia
Dentists frequently use this anesthetic combination to numb the gums before inserting a needle for local anesthesia during dental procedures, ensuring a pain-free experience.
3.4 Use in Minor Surgical Procedures
Lidocaine/Prilocaine is used before minor surgical interventions such as biopsies or the removal of superficial lesions, providing effective localized anesthesia with minimal systemic absorption.
3.5 Use in Chronic Pain Management
Though not its primary indication, the combination can be used to manage localized chronic pain conditions, such as peripheral neuropathy, due to its potent anesthetic properties.
4. Off-Label Uses of Lidocaine/Prilocaine
4.1 Off-Label Use in Postherpetic Neuralgia
Some practitioners use Lidocaine/Prilocaine off-label to treat postherpetic neuralgia, a chronic pain condition that follows shingles outbreaks. This provides temporary relief in affected areas.
4.2 Off-Label Use in Hemorrhoids Treatment
For patients suffering from painful hemorrhoids, Lidocaine/Prilocaine cream is occasionally used off-label to provide symptomatic relief by numbing the perianal region.
4.3 Off-Label Use in Sexual Health: Premature Ejaculation
Lidocaine/Prilocaine is used off-label in some topical formulations designed to treat premature ejaculation. It numbs the penile skin, delaying ejaculation by reducing sensitivity.
4.4 Other Experimental Uses
Researchers are exploring additional off-label uses for this combination, including its potential in treating conditions like vulvodynia and interstitial cystitis, although evidence is still being gathered.
5. How Lidocaine/Prilocaine Works
5.1 Mechanism of Action: Local Anesthetic Effects
Lidocaine/Prilocaine functions by inhibiting the conduction of nerve impulses in the targeted area. The sodium channel blockade prevents the propagation of pain signals to the brain.
5.2 Nerve Blockage and Pain Signal Inhibition
By creating a temporary blockade of sodium ions, the drugs halt the action potential required for nerve signals, effectively inducing a state of reversible numbness.
5.3 Onset of Action and Duration
The onset of numbness typically occurs within 30 to 60 minutes of application, depending on the thickness of the skin and the formulation used. The anesthetic effect generally lasts for 1 to 2 hours.
5.4 Factors Affecting Efficacy
Efficacy can vary based on skin type, dosage applied, and the area of application. Skin that is thicker or more resilient may require a longer time for the anesthetic to take full effect.
6. Dosage and Administration of Lidocaine/Prilocaine
6.1 Recommended Dosages for Different Procedures
For dermal anesthesia, the standard dose is a thin layer of cream applied to the area, typically 2.5 grams for 10 square centimeters of skin. For larger areas, adjustments are made accordingly.
6.2 Proper Application Methods (Creams and Patches)
When using creams, a thick layer should be applied and covered with an occlusive dressing for optimal absorption. Patches are applied directly to the skin without additional covering.
6.3 Frequency of Use and Duration of Treatment
Typically, Lidocaine/Prilocaine is used once for a procedure. In the case of chronic pain, reapplication may be necessary, though prolonged use should be closely monitored.
6.4 Special Considerations for Sensitive Skin Areas
When applying to sensitive areas such as the face or genitals, care must be taken to use appropriate doses to avoid excessive numbing or irritation.
6.5 How to Measure and Apply Dosage
Dosing should be measured based on the surface area. Commercial formulations often come with specific instructions for how much cream or gel to use per square centimeter of skin.
7. Side Effects of Lidocaine/Prilocaine
7.1 Overview of Common Side Effects
Common side effects of Lidocaine/Prilocaine are typically localized to the area of application and are temporary. These may include mild irritation, itching, or a burning sensation.
7.2 Skin Reactions (Redness, Itching, Rash)
Topical application may cause skin reactions such as redness or itching. These reactions are usually mild and resolve quickly without intervention.
7.3 Systemic Reactions (Dizziness, Nausea)
Although rare, systemic absorption of Lidocaine/Prilocaine may lead to dizziness, nausea, or other signs of toxicity, especially in high doses.
7.4 Serious Side Effects Requiring Medical Attention
Severe side effects, such as methemoglobinemia, although rare, can occur. This condition reduces the oxygen-carrying capacity of the blood and requires immediate medical attention.
8. Common Side Effects of Lidocaine/Prilocaine
8.1 Mild Irritation at the Site of Application
Mild irritation at the site of application is one of the most frequently reported side effects of Lidocaine/Prilocaine. Patients may experience slight redness, warmth, or an itching sensation. These symptoms typically subside shortly after removal of the cream or patch. It is important to monitor the area to ensure that irritation does not escalate to more serious skin conditions.
8.2 Numbness or Tingling Sensation
A transient numbness or tingling sensation may occur in the treated area. While this effect is expected due to the anesthetic properties of Lidocaine/Prilocaine, it can sometimes linger longer than desired. In rare cases, this sensation might extend beyond the intended area, especially if the medication spreads to adjacent tissues.
8.3 Temporary Skin Discoloration
Temporary changes in skin color, including pale or bluish discoloration, can occur following the application of Lidocaine/Prilocaine. This side effect is usually benign and resolves without intervention. However, patients should be advised to report any prolonged or worsening discoloration.
8.4 Localized Swelling
Some patients may develop localized swelling in the area of application. This is typically a mild, self-limiting reaction but should be noted, particularly if accompanied by pain or significant discomfort. The swelling is usually due to localized irritation or minor allergic response.
9. Warnings and Precautions for Lidocaine/Prilocaine Use
9.1 Important Precautions Before Use
Before using Lidocaine/Prilocaine, healthcare providers must review the patient’s medical history. It is vital to assess for any known hypersensitivity to local anesthetics or amide-type drugs. Additionally, the skin should be intact; applying the medication to broken or damaged skin increases the risk of systemic absorption and subsequent toxicity.
9.2 Risk of Allergic Reactions and Sensitivity
Though rare, allergic reactions to Lidocaine/Prilocaine can occur. Symptoms may include hives, difficulty breathing, or swelling of the face, lips, tongue, or throat. Patients with a known history of drug sensitivities or dermatological conditions should be monitored closely for any adverse effects.
9.3 Use in Patients with Liver or Kidney Disease
Patients with hepatic or renal impairment may metabolize Lidocaine/Prilocaine differently, leading to an increased risk of toxicity. Dose adjustments or alternative anesthetic agents should be considered in these individuals to avoid potential complications.
9.4 Warnings Regarding High Doses
Administering high doses of Lidocaine/Prilocaine, particularly over large surface areas or for extended durations, can result in systemic toxicity. Symptoms may include central nervous system depression, seizures, or cardiac arrhythmias. For this reason, the lowest effective dose should always be used.
9.5 Proper Handling and Storage
It is crucial to handle Lidocaine/Prilocaine with care, avoiding contact with the eyes and mucous membranes. The medication should be stored at room temperature and away from direct sunlight. In addition, proper disposal protocols must be followed to prevent accidental ingestion by children or pets.
10. Contraindications for Lidocaine/Prilocaine
10.1 Patients with Known Allergy to Local Anesthetics
Lidocaine/Prilocaine is contraindicated in individuals with a known allergy to amide-type local anesthetics. Such allergies may manifest as skin reactions, respiratory difficulties, or anaphylactic shock, requiring immediate medical intervention.
10.2 Conditions with Increased Risk of Methemoglobinemia
Patients with a predisposition to methemoglobinemia, a condition where oxygen delivery to tissues is impaired, should avoid Lidocaine/Prilocaine. The use of this anesthetic combination can induce or exacerbate methemoglobinemia, leading to life-threatening hypoxia.
10.3 Contraindicated Medications
Certain medications, such as other local anesthetics or drugs known to interact with liver enzymes, are contraindicated with Lidocaine/Prilocaine due to the increased risk of systemic toxicity. A thorough medication review should be conducted before prescribing this anesthetic.
11. Interactions with Other Drugs
11.1 Medications That May Increase Toxicity
Drugs that inhibit cytochrome P450 enzymes, such as cimetidine, can slow the metabolism of Lidocaine/Prilocaine, increasing the risk of toxic effects. Concurrent use of these medications should be avoided or carefully monitored.
11.2 Drug Interactions with Other Local Anesthetics
Using Lidocaine/Prilocaine in conjunction with other local anesthetics can result in additive effects, increasing the risk of systemic toxicity. Caution must be exercised when layering multiple anesthetic agents.
11.3 Interaction with Anticoagulants and Blood Thinners
Patients on anticoagulant therapy, such as warfarin or heparin, may experience increased bruising or bleeding at the site of Lidocaine/Prilocaine application. The risk-benefit ratio should be carefully considered in these cases.
11.4 Interaction with Cardiac Medications
Lidocaine is known to interact with certain cardiac medications, particularly antiarrhythmics. These interactions can lead to altered cardiac conduction, necessitating close monitoring of heart rate and rhythm during treatment.
12. Lidocaine/Prilocaine Use in Special Populations
12.1 Administration to the Elderly: Adjustments and Monitoring
Elderly patients may have altered pharmacokinetics due to age-related changes in metabolism and excretion. Dosage reductions and close monitoring are recommended to minimize the risk of adverse effects in this population.
12.2 Safe Use in Pregnant Women
The use of Lidocaine/Prilocaine during pregnancy should be approached with caution. Although studies have shown that it does not significantly increase the risk of birth defects, it should only be used when absolutely necessary and under medical supervision.
12.3 Use in Nursing Mothers: Risk vs. Benefit
Lidocaine and Prilocaine are excreted in breast milk, but in minimal amounts. Nursing mothers should use the medication cautiously, ensuring that any application is limited and that the infant is monitored for signs of toxicity, such as excessive drowsiness or irritability.
12.4 Administration to Children: Pediatric Dosage Recommendations
Pediatric use of Lidocaine/Prilocaine requires careful dosing based on body weight and age. Due to the increased susceptibility of children to methemoglobinemia, the dose should be minimized, and application times should be strictly adhered to.
13. Overdosage of Lidocaine/Prilocaine
13.1 Signs and Symptoms of Overdosage
Overdosage of Lidocaine/Prilocaine can result in symptoms such as confusion, visual disturbances, tremors, or even seizures. In severe cases, cardiac arrest may occur. Immediate medical intervention is required to mitigate these life-threatening risks.
13.2 Immediate Actions and Treatment Options
In the event of overdosage, discontinuation of the drug is paramount. Supportive care, including oxygen therapy and intravenous fluids, should be administered. In cases of severe methemoglobinemia, intravenous methylene blue may be necessary.
13.3 Long-Term Effects of Overdose
While most patients recover fully from an overdose with prompt treatment, prolonged exposure to toxic levels of Lidocaine/Prilocaine may result in long-term neurological or cardiovascular damage. Follow-up care is essential to assess recovery.
14. Handling and Storage of Lidocaine/Prilocaine
14.1 Safe Handling Practices
Lidocaine/Prilocaine should be applied using protective gloves to prevent accidental exposure. After application, the hands should be thoroughly washed to prevent the spread of the anesthetic to unintended areas.
14.2 Proper Storage Conditions
Lidocaine/Prilocaine must be stored at room temperature, ideally between 20°C and 25°C (68°F to 77°F). Exposure to excessive heat or cold can degrade the efficacy of the medication. Always keep the product in its original packaging to avoid contamination.
14.3 Disposal of Unused Medication
Unused or expired Lidocaine/Prilocaine should be disposed of according to local regulations for hazardous waste. It should not be flushed down the toilet or poured into drainage systems. Safe disposal methods prevent accidental ingestion or exposure.