Amoxapine
- Introduction
- Uses
- Off-label Use
- How it Works
- Dosage and Administration
- Composition
- Side Effects
- Common Side Effects
- Interaction
- Warning
- Contraindication
- Careful Administration
- Important Precautions
- Administration to Elderly
- Administration to Pregnant Women and Nursing Mothers
- Administration to Children
- Overdosage
- Storage
- Handling Precautions
Introduction
Brief history and development of Amoxapine
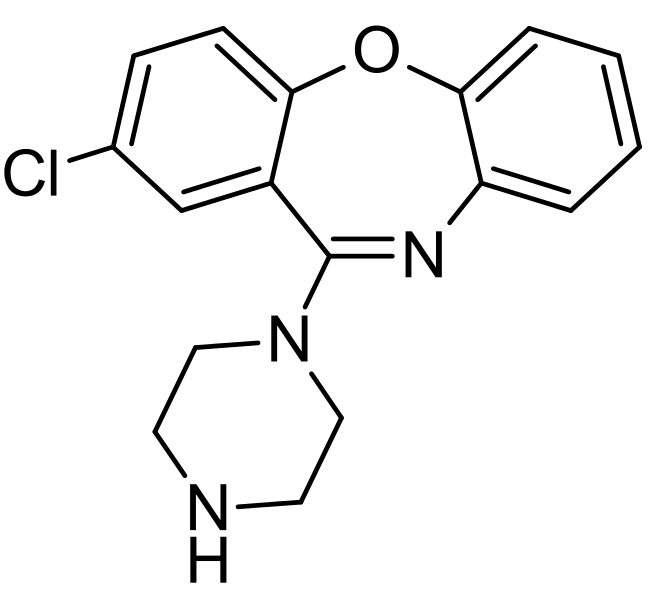
Amoxapine, a known medication belonging to the tricyclic antidepressant (TCA) group, dates back to the mid-20th century. It originated as a derivative of dibenzoxazepine. It started being used clinically in the late 1960s. Since then, it has found its place in treating individuals with depressive disorders, forming a specific niche within this patient population.
Overview of its place in the class of tricyclic antidepressants
Tricyclic antidepressants, known for their three-ring chemical structure, are considered one of the older categories of antidepressant medications. Amoxapine, in particular, has garnered attention for its ability to work on two fronts. Not only does it effectively inhibit the reuptake of serotonin and norepinephrine, but it also exhibits significant anti-dopaminergic activity.
Uses
Primary indications: Major depressive disorder and its manifestations
Amoxapine is primarily used to treat a condition called depressive disorder (MDD). This condition is characterized by an long lasting low mood and it can manifest in different ways, such as trouble sleeping or excessive sleeping significant changes in weight feelings of worthlessness or guilt difficulty concentrating and making decisions and recurrent thoughts of death or suicide. For people, with MDD Amoxapine provides hope by reducing these symptoms and enhancing their overall quality of life 1.
Benefits and outcomes for the major depressive disorder
Administering Amoxapine has shown results in reducing depressive symptoms among numerous patients. Clinical trials have highlighted improvements in mood, increased engagement in activities, and even enhanced sleep patterns. Moreover, compared to TCAs, Amoxapine often presents a favorable side effect profile, making it a viable choice for many patients.
Off-label Use
Anxiety disorders: Efficacy and studies supporting this use
Although Amoxapine is not typically prescribed for anxiety disorders, there is emerging evidence suggesting its therapeutic benefits in this area. Initial studies have shown that its strong serotonergic effects may help alleviate symptoms of anxiety disorder and specific phobic disorders 2. These preliminary findings open up possibilities for exploring the therapeutic applications of Amoxapine.
Sleep disorders: How Amoxapine may be beneficial
Although Amoxapine is not typically prescribed for sleep disorders, there are anecdotal reports suggesting that it could potentially reduce the time it takes to fall asleep and improve the overall quality of sleep for specific groups of individuals struggling with insomnia 2.
1: Medscape 2: PubMed
Neuropathic pain: Examining its potential effectiveness
Amoxapine is a tricyclic antidepressant that is primarily used to treat a condition called depressive disorder (MDD) 1. Although Amoxapine is not typically prescribed for neuropathic pain, there is growing evidence suggesting its potential in reducing pain, particularly in cases of post-herpetic neuralgia and diabetic neuropathy 2. Its ability to regulate neurotransmitters, specifically serotonin and norepinephrine, may be responsible for its pain-relieving properties. However, extensive clinical trials are needed to establish its effectiveness in managing neuropathic pain.
How it Works
Mechanism of action: Interaction with neurotransmitters
Amoxapine interacts with neurotransmitters in the brain, a crucial aspect of its mechanism. It increases the levels of serotonin and norepinephrine by preventing their reuptake, which has an impact on regulating mood. Moreover, it also acts as an antagonist of dopamine receptors, making it distinct from other tricyclic antidepressants and enhancing its therapeutic effects.
Comparison with other tricyclic antidepressants
Although Amoxapine shares the primary mechanism as other TCAs in boosting serotonin and norepinephrine, its anti-dopaminergic activity sets it apart. This unique feature often leads to a set of side effects, which makes Amoxapine a potential option for patients who may not be able to tolerate other TCAs.
Dosage and Administration
Recommended starting dose for adults
When adults are prescribed Amoxapine, starting with a daily dose of 50 to 75 mg is usually suggested. This can be taken in doses throughout the day or as a single dose in the evening. The dosage may be adjusted depending on how it works and how well it is tolerated.
Adjustments for specific populations
Certain population groups, such as the elderly or individuals with insufficiency, might require adjustments in their medication dosage. By initiating treatment with doses and closely monitoring their progress, we can prevent potential adverse effects in these populations.
Duration of treatment and discontinuation protocol
The length of time a patient should take Amoxapine depends on how they respond. Some individuals may require long-term treatment. It's vital to assess their progress regularly. It should be done gradually over a week if discontinuation is necessary to avoid any potential withdrawal symptoms.
Composition
Core ingredients in Amoxapine
The primary active component of Amoxapine is its dibenzoxazepine compound. This fundamental compound plays a role in its antidepressant and neuromodulatory effects.
Inactive ingredients and their roles
Amoxapine tablets also include a range of components, such as binding agents, fillers, and stabilizers. These extra substances help maintain the drug's effectiveness, improve its absorption into the body, and aid manufacturing and formulation processes.
Side Effects
Mild side effects: Overview and frequency
Some of the mild side effects experienced with Amoxapine include dryness in the mouth, blurry vision, constipation, weight gain, and fatigue. Generally, these effects are temporary. It tends to diminish as the body adjusts to the medication.
Severe side effects: Potential risks and their rarity
Although uncommon, adverse effects may arise, such as cardiac arrhythmias, severe hypotension, seizures, neutropenia, and serotonin syndrome. If any of these symptoms occur, seeking medical attention and considering adjusting or discontinuing the medication if necessary is essential.
Common Side Effects
Most frequently reported symptoms by patients
Patients commonly experience symptoms such as dizziness, feeling sleepy, and having a mouth. These effects are usually harmless. Tend to improve as the treatment progresses or with slight adjustments in the dosage.
Management and mitigation strategies
To address the reactions, methods like lowering the dosage using additional treatments or making simple changes to one's lifestyle, such as drinking more water for a dry mouth, can be helpful. Consistently educating patients and closely monitoring their progress are also factors in achieving the best treatment results while minimizing adverse effects.
Interaction
Common drugs that can interfere with Amoxapine's effectiveness
When prescribing Amoxapine, paying attention to possible interactions with other medications is crucial. There are common culprits that you should be aware of: MAO inhibitors. These can cause severe episodes of high blood pressure. Anticholinergics: They may have effects on anticholinergic activity. Cimetidine: This medication could potentially increase the levels of Amoxapine in the body. SSRIs can potentially elevate levels, which may put the patient at risk for serotonin syndrome. Barbiturates: They could possibly lower the levels of Amoxapine in the bloodstream. It is essential to be cautious and monitor for any drug interactions when prescribing Amoxapine.
Potential results of these interactions
The effectiveness of amoxapine treatment can be weakened by drug interactions, leading to increased side effects or adverse reactions. These interactions can range from drowsiness to severe serotonin syndrome, highlighting the importance of careful monitoring and control over medication use.
Warning
Serious potential outcomes and risk factors
Although it has benefits, Amoxapine carries the risk of severe consequences such as Torsades de pointes. This is a life-threatening heart rhythm disorder. Symptoms like restlessness, hallucinations, and a rapid heartbeat can identify serotonin syndrome. Neutropenia refers to a decrease in white blood cells—seizures, especially in cases of excessive dosage.
Monitoring and early detection methods
It is crucial to monitor the heart, conduct blood tests, and assess neurological functions. These surveillance techniques are essential for identifying and addressing the risks mentioned earlier.
Contraindication
Conditions or situations where Amoxapine should not be used
Amoxapine should not be used in situations, including When taking MAO inhibitors simultaneously or within two weeks after stopping them. During the acute recovery phase following a heart attack. If you have narrow-angle glaucoma.
Alternative treatments for those with contraindications
Patients who should not take Amoxapine may want to explore treatment options such as SSRIs, newer antipsychotics, or psychotherapy after undergoing a thorough medical evaluation.
Careful Administration
Situations requiring dosage adjustments
The dosage of Amoxapine may need adjustment in cases of liver problems, kidney insufficiency, or when taken together with CYP450 inhibitors.
Monitoring for specific side effects or interactions
It is crucial to monitor individuals, particularly when taking medications with sedative, anticholinergic, or QT-prolonging effects. In these situations, doctors often request electrocardiograms (ECGs), liver function tests, and renal panels.
Important Precautions
Steps for safe administration
To ensure safety, begin with the lowest dose that is still effective. It's essential to avoid consuming alcohol or any other substances that can depress the nervous system. Abruptly stopping the medication should be avoided. It is crucial to remain vigilant for any signs of thoughts, particularly during the drug's initial stages.
Recommendations for regular health check-ups
Regular checkups, heart health blood tests, and mental health assessments can help identify any issues ahead of time, making the treatment process safer.
Administration to Elderly
Dose considerations and modifications
For patients, it is advisable to begin with a lower dosage and gradually increase it while carefully monitoring for any adverse effects. This approach is recommended to ensure safety and well-being.
As people get older, they become more susceptible to hypotension, cognitive problems, and difficulty with urination. It can be helpful to monitor blood pressure, conduct tests, and observe urinary patterns in this age group.
Administration to Pregnant Women and Nursing Mothers
Research and potential risks during pregnancy
While there is research on the effects of Amoxapine during pregnancy in humans, animal studies indicate possible risks to the unborn baby. Evaluating whether the benefits of taking Amoxapine outweigh any potential risks before using it during gestation is essential.
Considerations for breastfeeding while on Amoxapine
Considering that Amoxapine and its byproducts may be passed on to breast milk, it is essential to consider the potential adverse effects on infants. Seeking advice from a pediatrician and a psychiatrist can provide insights for making an informed decision.
Administration to Children
Safety profile and age limits
The safety of Amoxapine in children is still not fully understood. It should be prescribed cautiously and when there are clear benefits.
Dose adjustments and considerations for pediatric patients
If it is considered necessary, starting with amounts, closely monitoring and adjusting based on how effective and well tolerated it is can help reduce any potential risks when dealing with children.
Overdosage
Symptoms of Amoxapine overdose
Overdosing can result in health complications, including irregular heartbeats, decreased central nervous system functioning, difficulty in breathing, seizures, and abnormally high body temperature.

Emergency treatment and management strategies
Getting help right away is crucial. It's essential to consider treatments, like lavage, giving activated charcoal and providing supportive care to manage symptoms. Sometimes, intensive care unit admission may be necessary to save a person's life.
Storage
Ideal storage conditions for Amoxapine
Keep it in a dry area away from direct sunlight and at temperatures below 25°C. Make sure to keep it out of the reach of children and pets.
Shelf life and disposal recommendations
Usually, Amoxapine remains effective for three years after it has been manufactured. It is essential to dispose of expired medications by utilizing pharmacy take-back programs or following local regulations.
Handling Precautions
Proper handling and dispensing of Amoxapine
When working with Amoxapine, wearing gloves, avoiding contact with the skin, and ensuring that the medication is stored in child-resistant containers is essential. Additionally, remember to provide patients with the patient information leaflet provided by the manufacturer.
Recommendations for health professionals and caregivers
Ongoing learning about the characteristics of the medication, possible adverse reactions, and the significance of following it can empower patients to have a better understanding and safer experience with their treatment. Listening to patient input and making any necessary adjustments to their treatment plans is essential.


















